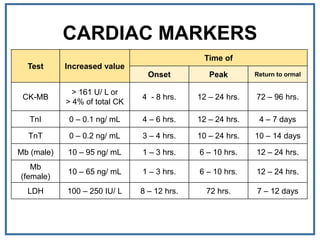
This document discusses various cardiac biomarkers used to detect myocardial injury, including troponins, CK-MB, myoglobin, and heart-type fatty acid binding protein. It provides details on each biomarker such as when levels increase after a cardiac event, peak time, and return to normal. Additional biomarkers discussed include ischemia modified albumin, high-sensitivity C-reactive protein, and natriuretic peptides. The document provides context on interpreting biomarker levels for assessing cardiac versus muscular injury.



































![OXIDIZED LDL
• Oxidized LDL has been attributed a key role in the
development of atherosclerosis.
• Several methods have been used to measure it, but they
yield potentially different data.
• Some have correlated malondialdehyde LDL with the
development of atherosclerosis and short-term events.
• Direct identification with antibodies suggests that oxidized
LDL may be released from vessels and may colocalize with
lipoprotein a [Lp(a)] after acute events.](https://image.slidesharecdn.com/cardiacbiomarkers-ii-180919215920/85/Cardiac-biomarkers-II-39-320.jpg)

![MATRIX METALLOPROTEINASES
• Matrix metalloproteinases (MMPs) can degrade the collagen matrix in coronary
artery or myocardium.
• They are integral to remodeling of the coronary artery and/or the heart after
acute events.
• Elaboration of MMP-9, a gelatinase, is thought to be important in plaque
destabilization; thus some have tried to measure it as a prognostic index.
• Other MMPs participate in the elaboration of extracellular matrix in the heart.
• Many MMPs also have inhibitors [tissue inhibitors of metalloproteinase
(TIMPs)] that modulate their effects.
• At present, standardized assays, reference intervals studies, and
• consistent assay validations are not available.](https://image.slidesharecdn.com/cardiacbiomarkers-ii-180919215920/85/Cardiac-biomarkers-II-41-320.jpg)






