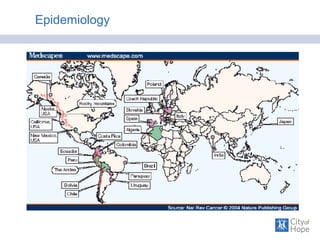
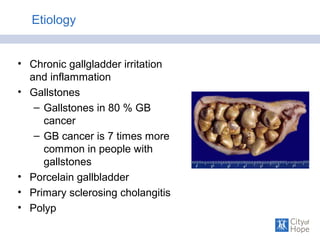
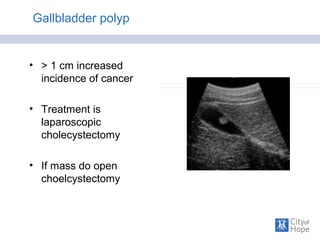
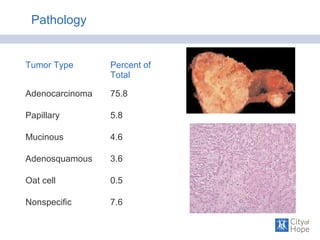
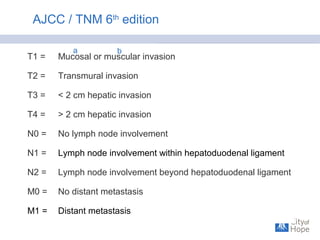
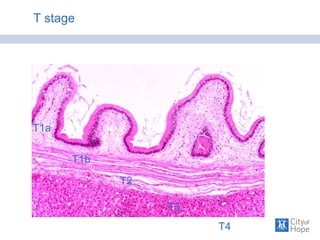
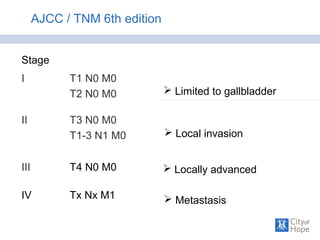
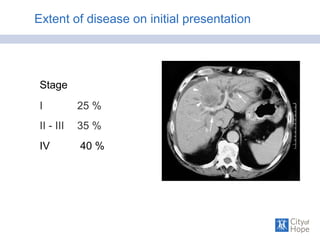
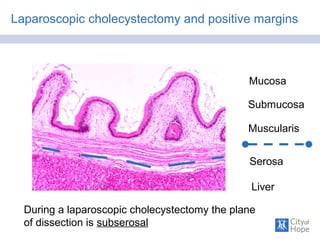
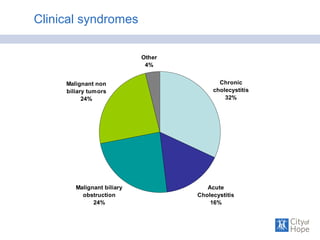
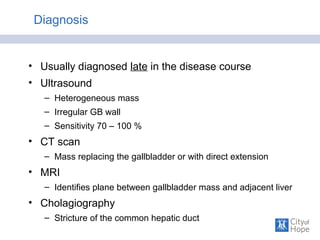
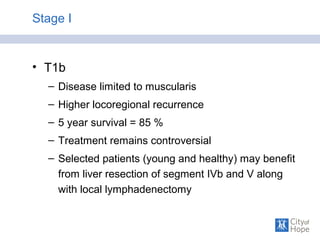
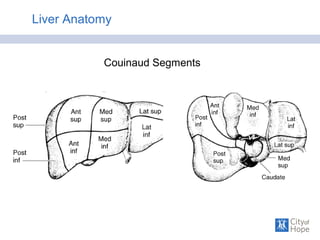
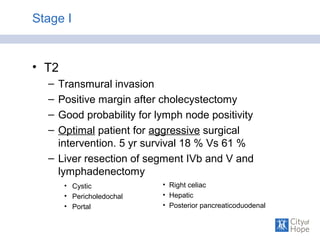
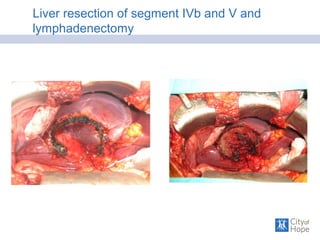
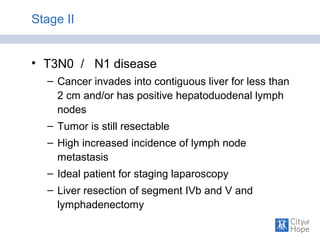
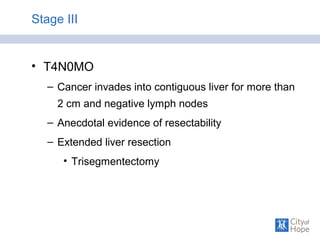
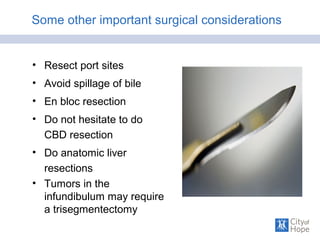
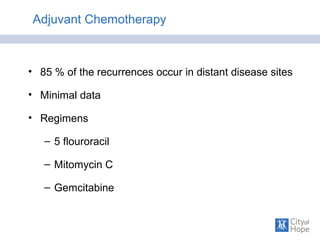
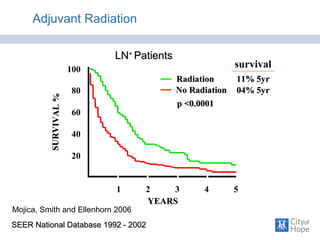
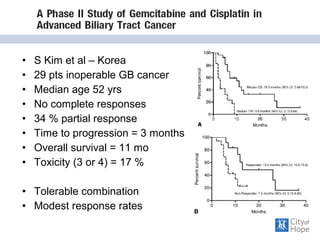
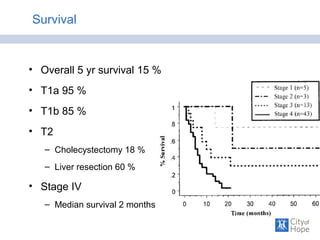
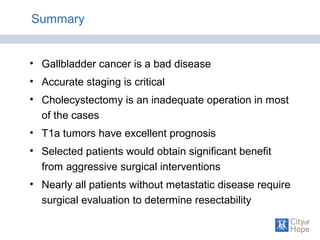
This document summarizes the surgical aspects of treating gallbladder cancer. It discusses the epidemiology, risk factors, staging, diagnosis, and management of gallbladder cancer. For early stage I tumors, surgery including cholecystectomy is usually sufficient. For more advanced stages II-III, aggressive surgery involving liver resection and lymphadenectomy may improve survival rates. Stage IV cancer with metastases has a very poor prognosis with chemotherapy and palliation the only options. An aggressive surgical approach can benefit carefully selected patients without metastatic disease.