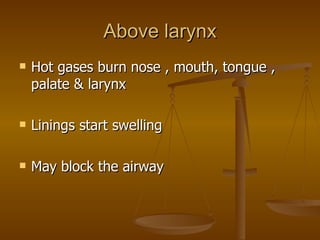
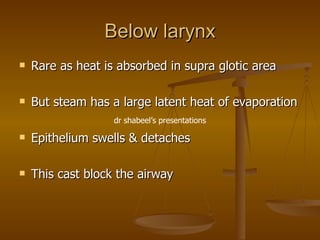
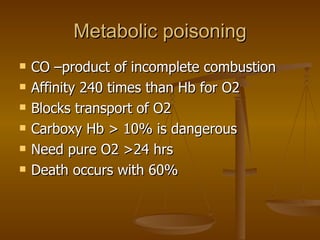
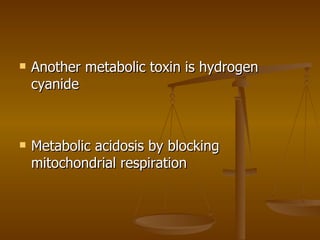
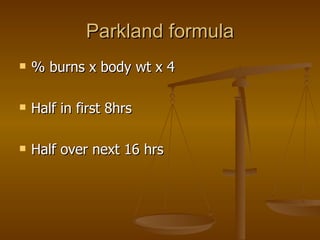
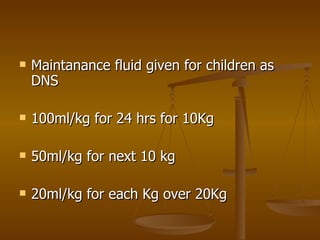
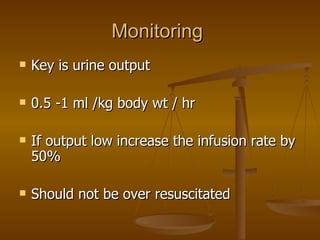
The document discusses the epidemiology, assessment, treatment and management of burns. It notes that the majority of burns in children are scalds, while flame burns are more common in adults. Assessment involves determining the percentage of total body surface area burned and burn depth. Treatment includes fluid resuscitation, wound care using dressings like silver sulfadiazine, and management of complications like inhalation injury and infection. Good outcomes depend on factors like percentage and depth of burns, and presence of an inhalation injury.