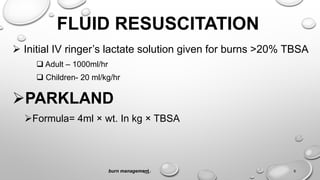
This document provides information on the management of burn injuries. It discusses pre-hospital care including stopping the burning process, assessing ABCs, and transporting the patient. It also outlines hospital care such as the primary survey assessing airway, breathing, circulation, exposure and secondary survey. Fluid resuscitation is discussed including formulas for calculating fluid needs. Wound care including cleaning, debridement and topical treatments is explained. Procedures like escharotomy and skin grafts are also summarized. Overall, the document provides guidance on assessing and treating burn patients in both pre-hospital and hospital settings.