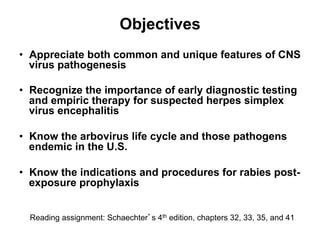
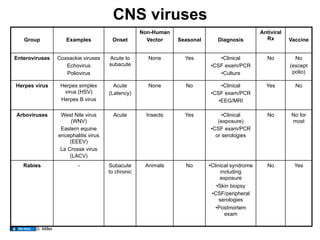
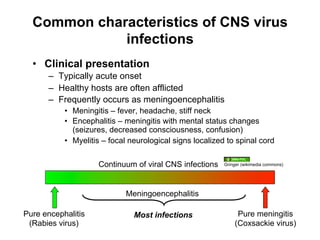
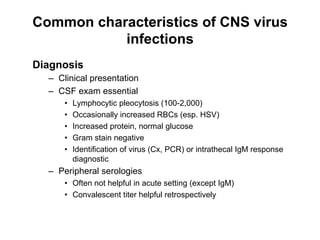
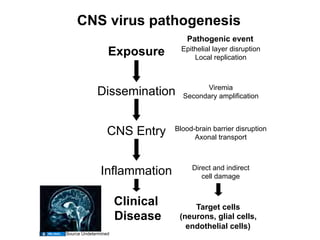
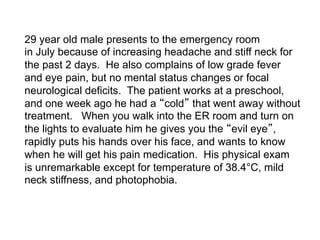
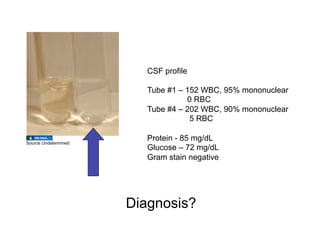
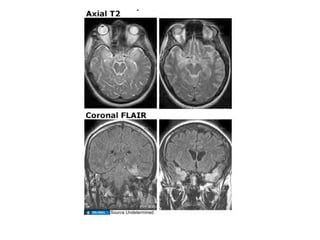
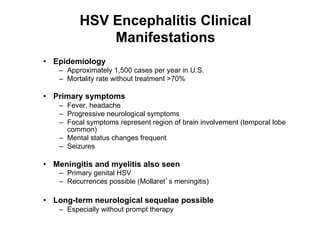
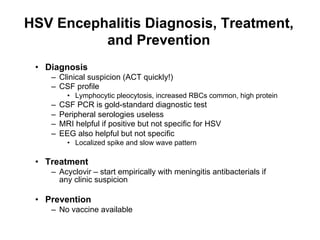
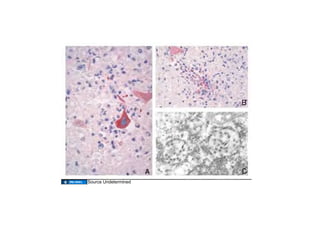
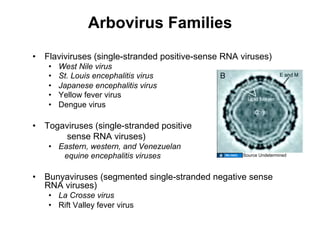
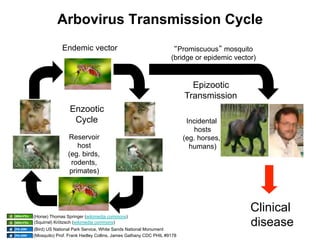
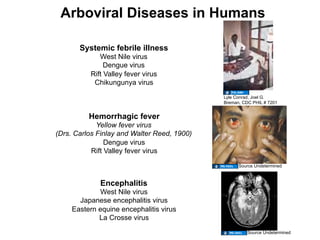
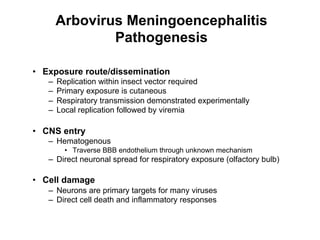
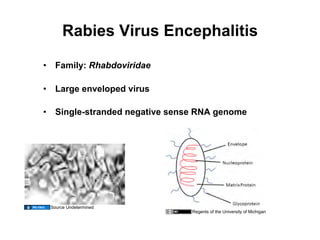
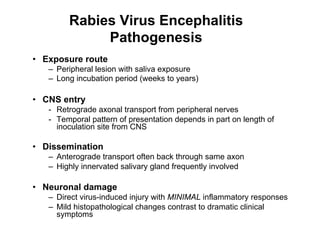
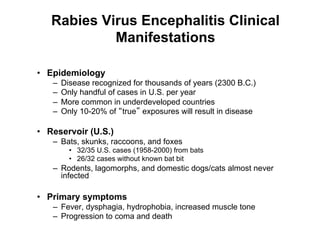
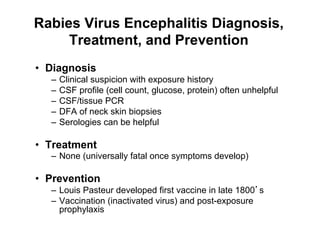
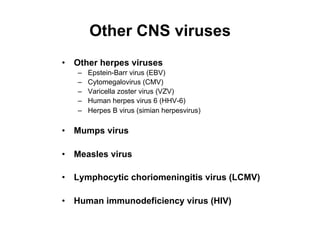
The document discusses various central nervous system (CNS) viral infections, focusing on their pathogenesis, common clinical presentations, diagnostic methods, and treatments. It emphasizes the need for early diagnostic testing and treatment, particularly for conditions like herpes simplex virus encephalitis and arbovirus infections. The document also highlights the potential public health implications and the importance of understanding these viruses in the context of epidemiology and patient care.