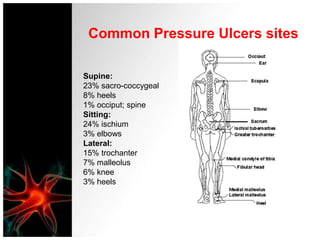
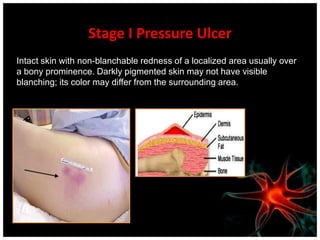
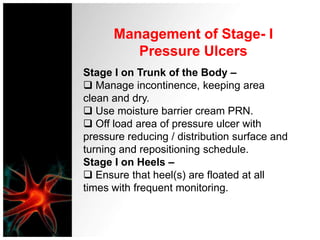
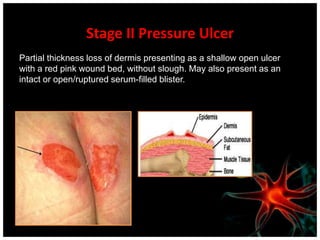
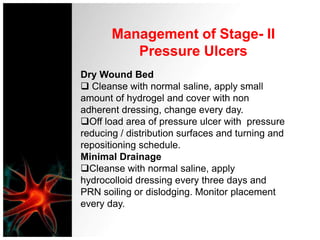
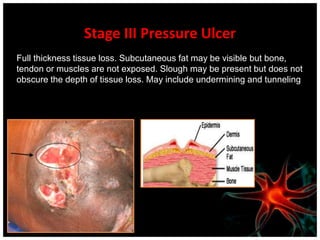
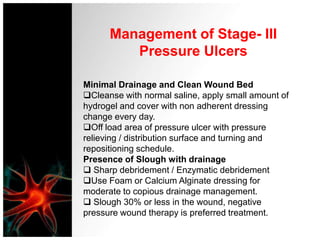
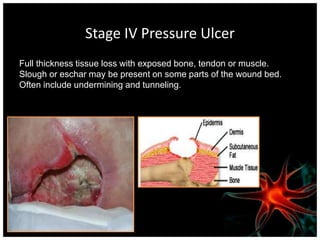
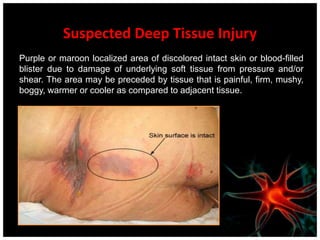
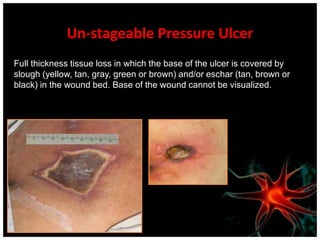
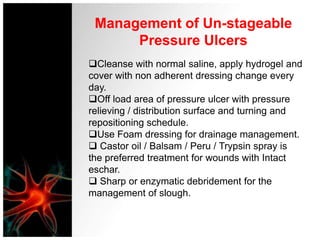
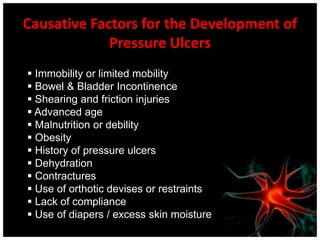
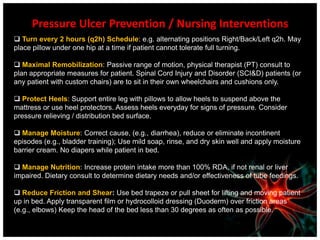
This document provides information on pressure ulcer assessment and management. It defines pressure ulcers and describes the common sites where they occur. It also outlines the classification system for staging pressure ulcers from Stage I to IV, as well as categories for suspected deep tissue injury and unstageable ulcers. For each stage and category, the document details approaches for assessment, wound cleaning, debridement if needed, dressing selection, and offloading of pressure. It lists causative factors for pressure ulcer development and nursing interventions for prevention.