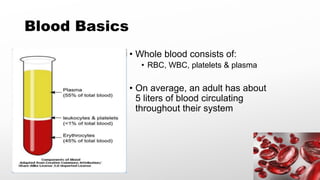
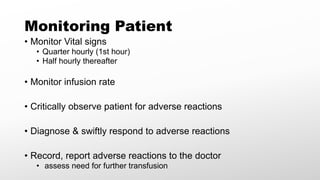
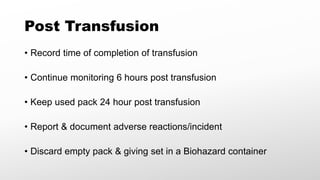
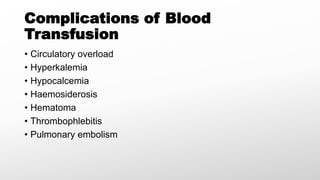
This document provides guidance on proper blood transfusion practices to ensure safe and effective transfusions. It outlines the basics of blood and its components, the decision process for transfusions, how to order and deliver blood to patients, pre-administration checks, monitoring patients during and after transfusions, and potential complications. The overall aim is to promote qualified practitioners following proper collection, administration, and monitoring procedures to minimize risks to patients.