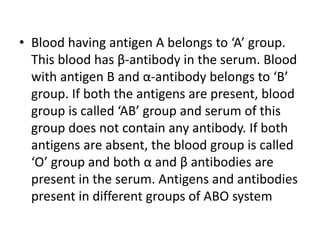
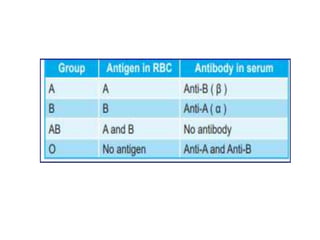
Karl Landsteiner discovered the ABO blood group system in 1901 and was honored with the Nobel Prize for this discovery in 1930. He found that blood can be categorized into four main groups - A, B, AB, and O - depending on the presence or absence of antigens A and B on red blood cells. The ABO system is important for blood transfusions, as transfusing incompatible blood can cause agglutination of red blood cells and transfusion reactions. Proper matching of donor and recipient blood types is essential to ensure safe transfusions.