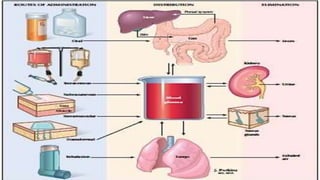
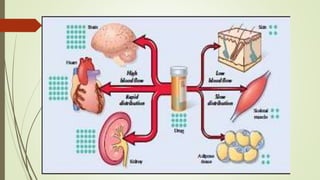
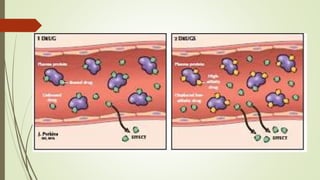
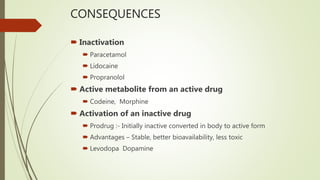
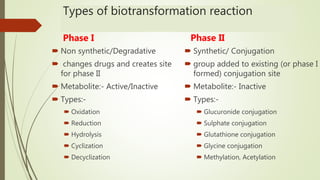
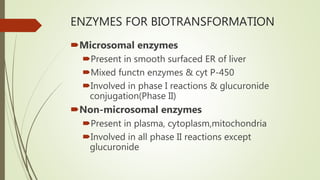
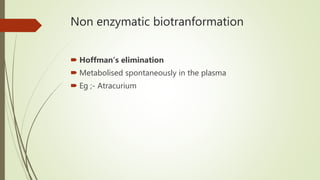
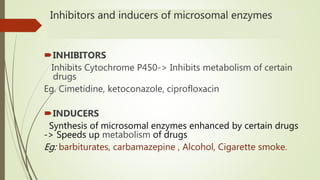
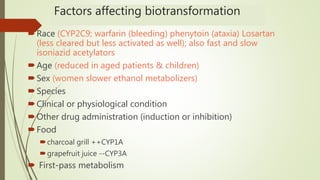
The document discusses biotransformation, which is the chemical alteration of drugs in the body. The body treats drugs as foreign substances and converts them into more polar, water soluble compounds through biotransformation so they can be excreted through the kidneys. Biotransformation occurs primarily in the liver and involves two phases - phase I reactions change the drug through processes like oxidation and phase II involves conjugating the drug to make it inactive so it can be excreted. Factors like other drugs, food, and an individual's characteristics can impact the biotransformation of drugs through inhibition or induction of the enzymes involved.