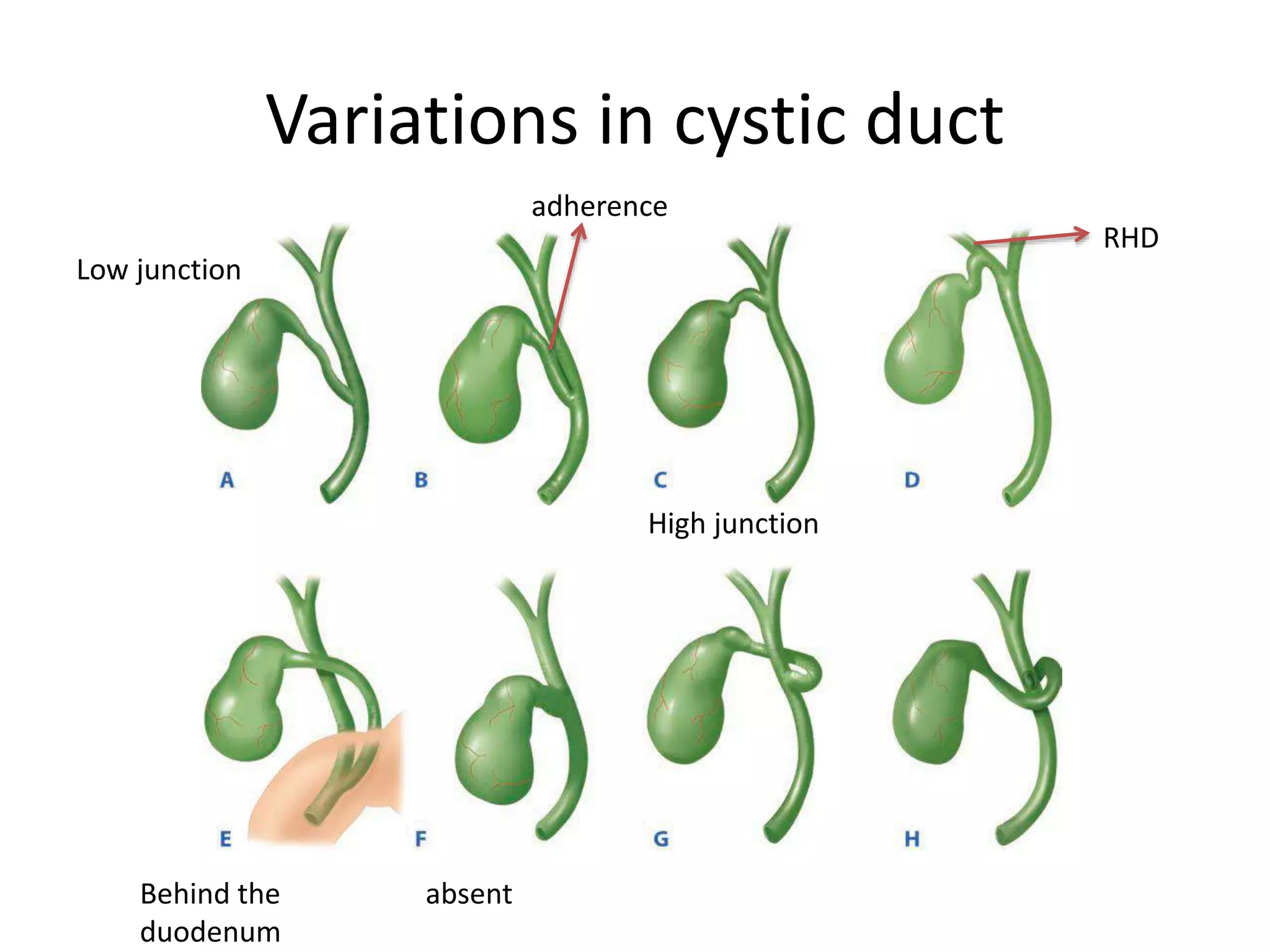
This document provides an overview of the anatomy, physiology, and investigations of the biliary system. It describes in detail the anatomy of structures including the gallbladder, cystic duct, hepatic ducts, common hepatic duct, common bile duct, and sphincter of Oddi. Key aspects of biliary system physiology such as enterohepatic circulation and defects that can occur are summarized. Common investigations for evaluating the biliary system including blood tests, imaging modalities like ultrasound, CT, MRI, and functional studies like HIDA scan are covered in brief.