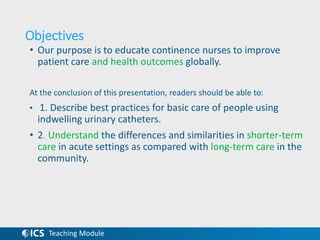
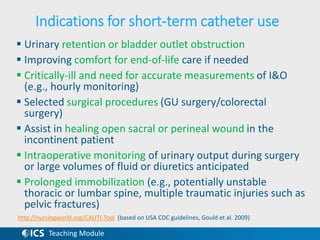
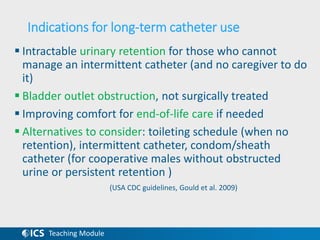
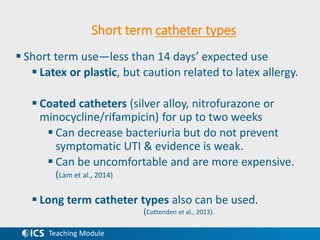
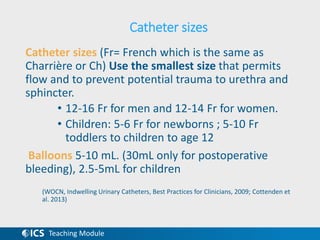
This document provides information on best practices for basic care of indwelling urinary catheters. It discusses short-term versus long-term catheter use, types of catheters, insertion and securement, drainage bags, irrigation, symptoms of catheter-associated urinary tract infections, and prevention of CAUTIs. The document aims to educate continence nurses to improve patient care and health outcomes related to indwelling urinary catheter use globally.
















![Teaching Module
• Glynn A, Ward V, Wilson J, et al. 1997. Hospital Acquired
Infection: Surveillance Policies and Practice. A Report of a Study of
the Control of Hospital Acquired Infection in 19 Hospitals in
England and Wales. London: Public Health Laboratory Service.
• Gould, C. V., Umscheid, C. A., Agarwal, R. K., Kuntz, G., Pegues, D.
A., & and the Healthcare Infection Control Practices Advisory
Committee (HICPAC). (2009). Guideline for prevention of catheter-
associated urinary tract infections 2009. Atlanta, GA: Centers for
Disease Control and Prevention.
• Jahn, P., Beutner, K., & Langer, G. (2012). Types of indwelling
urinary catheters for long-term bladder drainage in adults. The
Cochrane Database of Systematic Reviews, 10, CD004997.
doi:10.1002/14651858.CD004997.pub3 [doi]
• Kunin, C. M., & McCormack, R. C. (1966). Prevention of catheter-
induced urinary-tract infections by sterile closed drainage. The
New England Journal of Medicine, 274(21), 1155-1161.
doi:10.1056/NEJM196605262742101](https://image.slidesharecdn.com/bestpracticesindwellingcathetersjan-230327150429-00a831eb/85/Best_Practices_Indwelling_catheters_Jan-14-16-pptx-24-320.jpg)
![Teaching Module
• Lo, E., Nicolle, L. E., Coffin, S. E., Gould, C., Maragakis, L. L.,
Meddings, J., . . . Yokoe, D. S. (2014). Strategies to prevent
catheter-associated urinary tract infections in acute care
hospitals: 2014 update. Infection Control and Hospital
Epidemiology, 35 Suppl 2, S32-47.
• Lam, T. B., Omar, M. I., Fisher, E., Gillies, K., & MacLennan, S.
(2014). Types of indwelling urethral catheters for short-term
catheterisation in hospitalised adults. The Cochrane Database
of Systematic Reviews, 9, CD004013.
doi:10.1002/14651858.CD004013.pub4 [doi]
• Moore, K.N., Hunter, K.F., McGinnis, R., Puttagunta, L,
Chobanak, J., Bascu, C., Fader M., & Voaklander, D. (2009). Do
catheter washouts extend patency time in long term urethral
catheters? A randomized controlled trial of acidic washout
solution, normal saline washout, or standard care. Journal of
Wound, Ostomy and Continence Nursing, 36, 82-90.](https://image.slidesharecdn.com/bestpracticesindwellingcathetersjan-230327150429-00a831eb/85/Best_Practices_Indwelling_catheters_Jan-14-16-pptx-25-320.jpg)
![Teaching Module
• Parkin, J., Scanlan, J., Woolley, M., Grover, D., Evans, A., & Feneley, R.
C. (2002). Urinary catheter 'deflation cuff' formation: Clinical audit
and quantitative in vitro analysis. BJU Int, 90(7), 666-71.
• Siegel, T. J. (2006). Do registered nurses perceive the anchoring of
indwelling urinary catheters as a necessary aspect of nursing care?: A
pilot study. J Wound Ostomy Continence Nurs, 33(2), 140-4.
• Wilde, M. H. (1986). Living with a Foley. American Journal of Nursing ,
86(10), 1121-3.
• Wilde, M. H., Brasch, J., Getliffe, K., Brown, K. A., McMahon, J. M.,
Smith, J. A., . . . Tu, X. (2010). Study on the use of long-term urinary
catheters in community-dwelling individuals. Journal of Wound,
Ostomy, and Continence Nursing, 37(3), 301-310.
doi:10.1097/WON.0b013e3181d73ac4
• Wilde, M. H., Fader, M., Ostaszkiewicz, J., Prieto, J., & Moore, K.
(2013). Urinary bag decontamination for long-term use: A systematic
review. Journal of Wound, Ostomy, and Continence Nursing, 40(3),
299-308. doi:10.1097/WON.0b013e3182800305 [doi]](https://image.slidesharecdn.com/bestpracticesindwellingcathetersjan-230327150429-00a831eb/85/Best_Practices_Indwelling_catheters_Jan-14-16-pptx-26-320.jpg)
