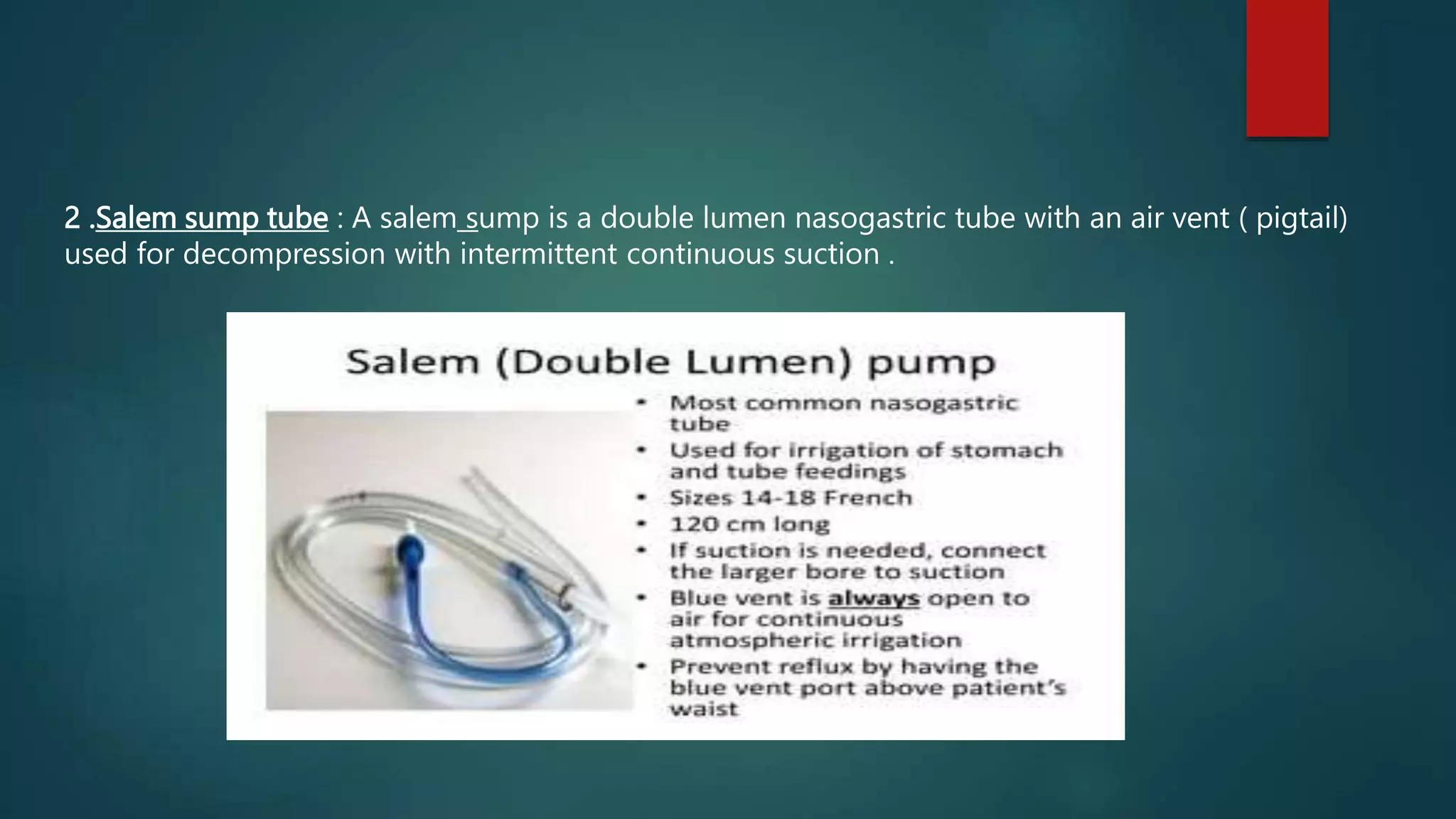
This document provides instructions for nasogastric tube insertion and feeding. It discusses the purposes of nasogastric tubes, types of tubes, tube insertion procedures, administration of feedings through the tubes, and precautions to take. Tube insertion involves measuring the tube's length and lubricating and inserting it into the stomach. Feedings are administered after checking tube placement and residual amounts. Precautions are outlined to prevent complications like diarrhea, aspiration, clogged tubes, and vomiting.