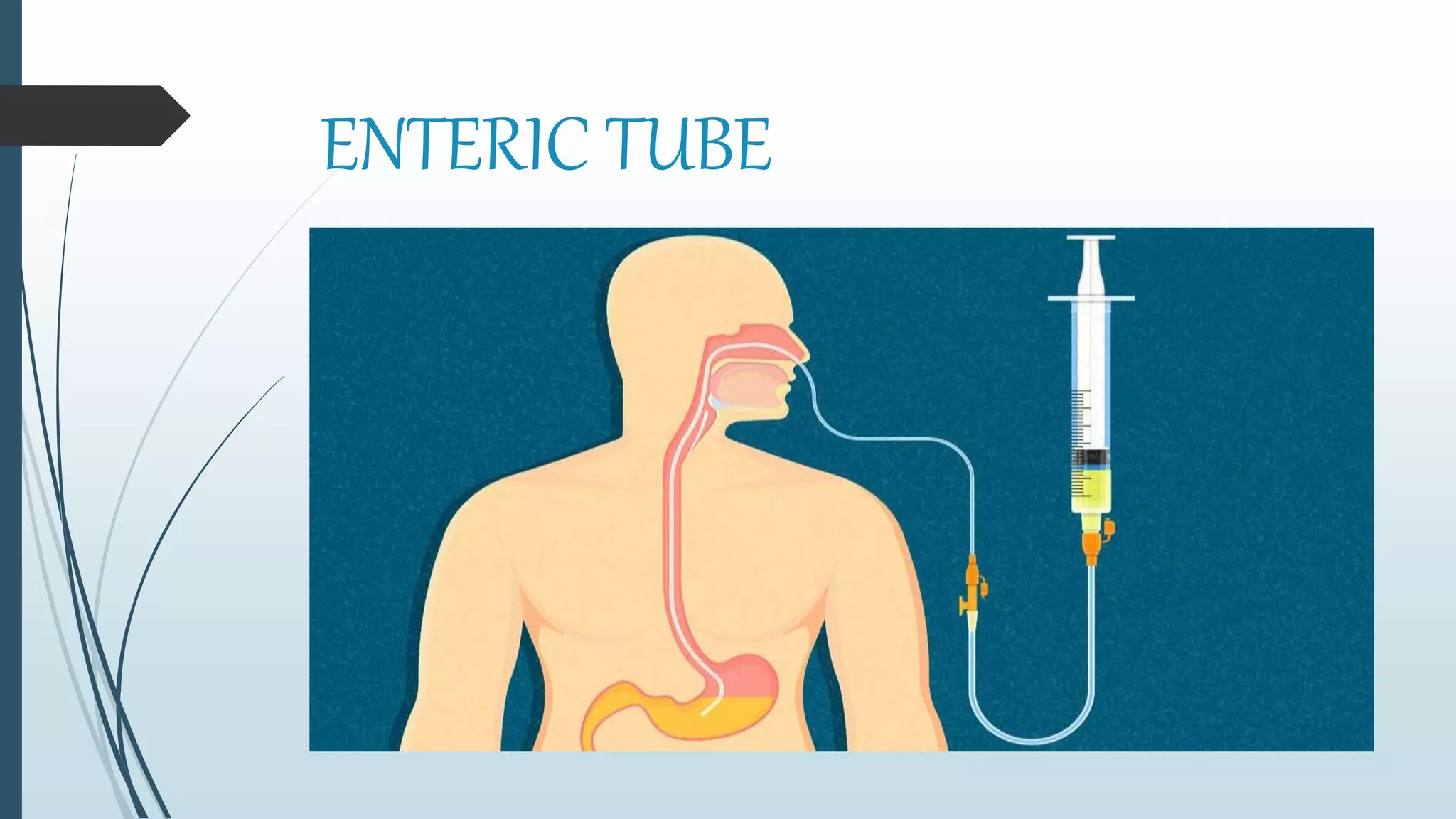
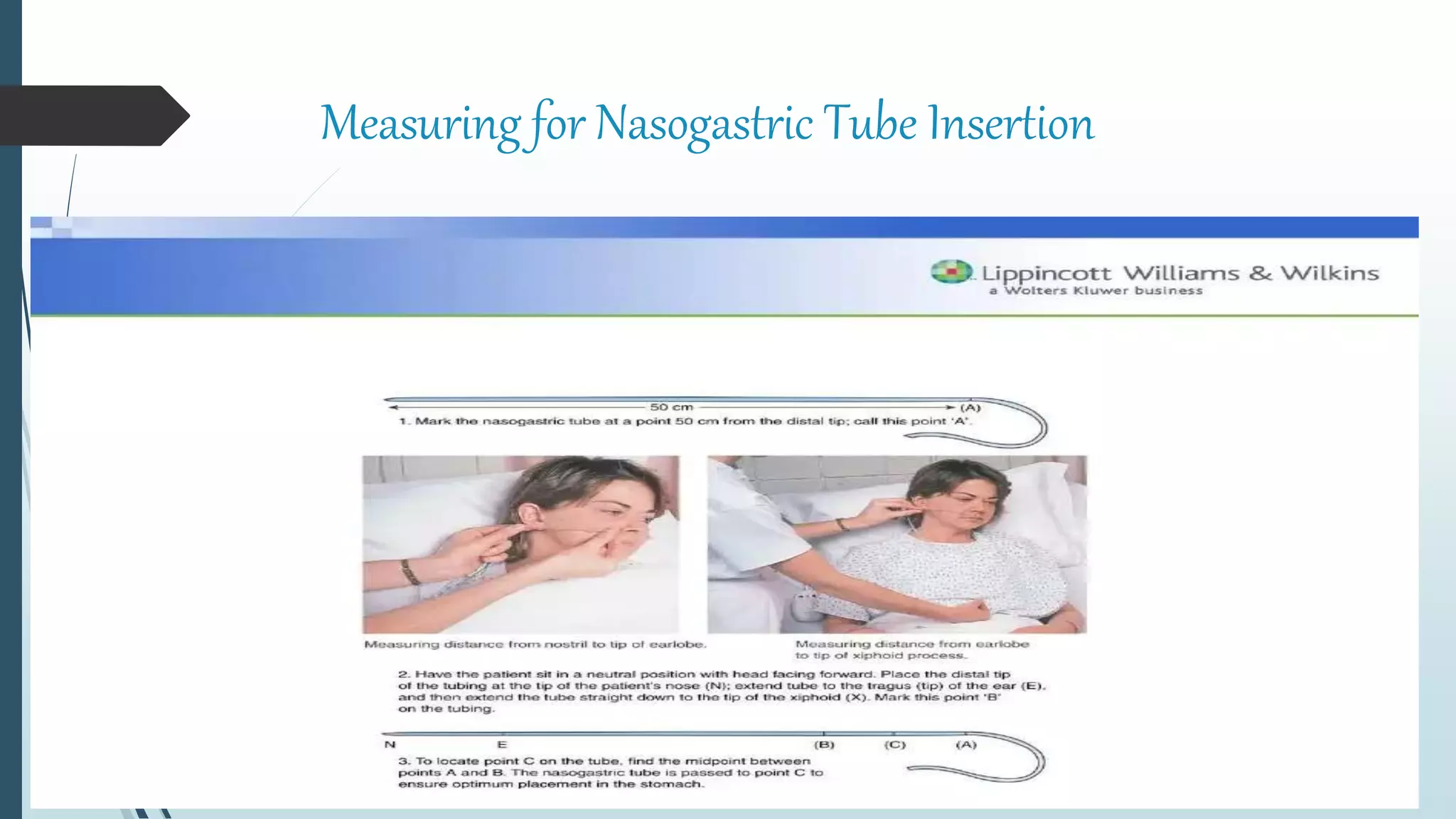
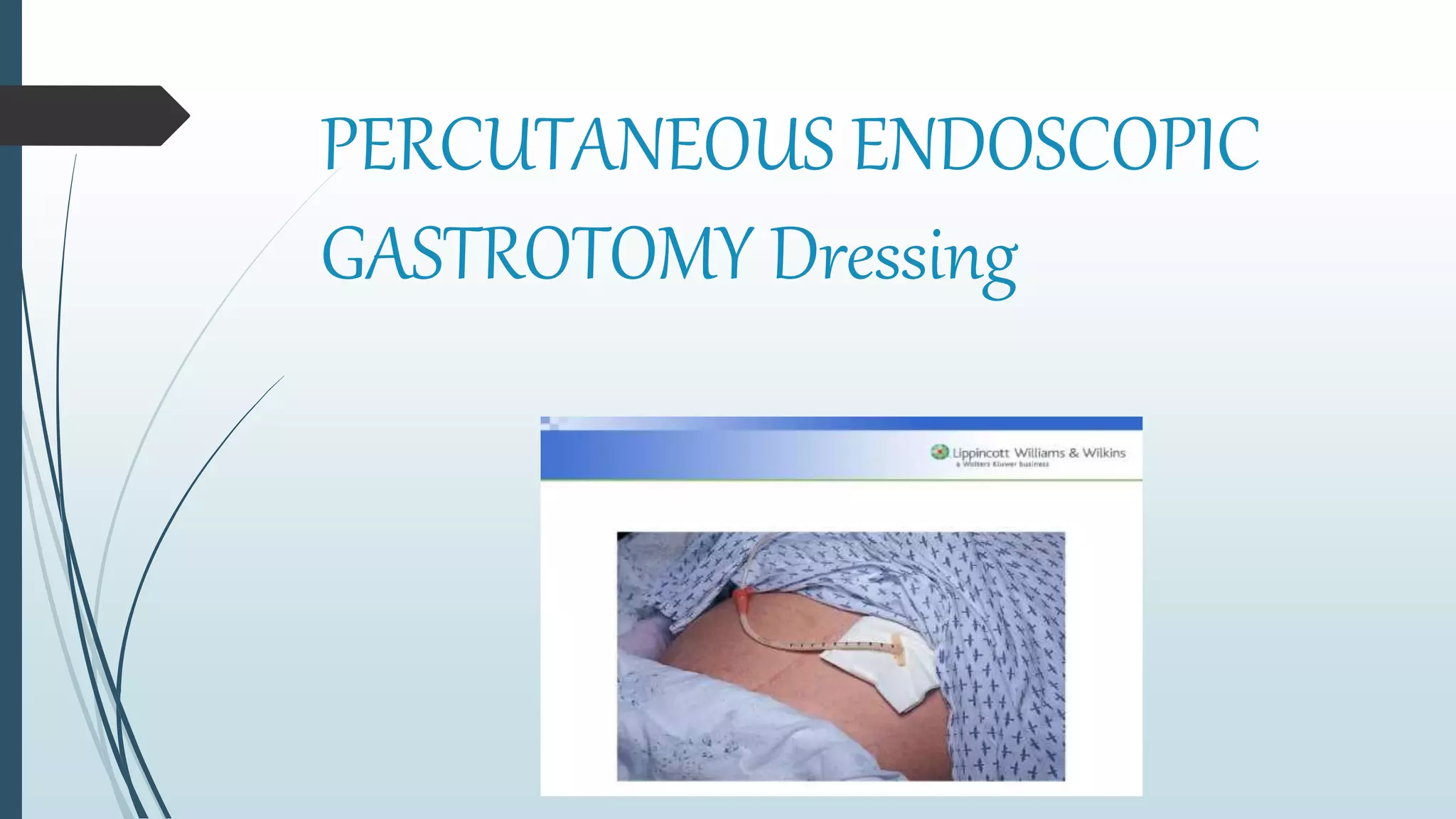
This document discusses various gastrointestinal intubation procedures and techniques. It defines gastrointestinal intubation as the insertion of flexible tubes into the stomach or small intestine for various purposes like decompressing the stomach, administering medications, or treating an obstruction. The document describes different types of tubes that can be used including gastric tubes, Levin tubes, sump tubes, and enteric tubes. It provides details on nursing care responsibilities for patients with nasogastric or gastrostomy tubes, including tube insertion and maintenance, assessing for complications, and providing patient education.