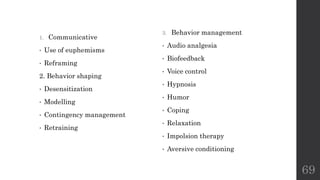
The document provides an overview of non-pharmacological behavior management techniques for children in dental settings. It discusses:
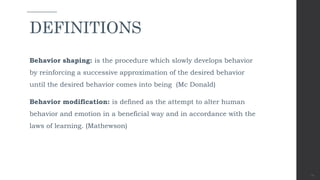
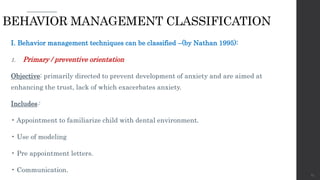
1) Definitions of key terms like behavior shaping and behavior modification.
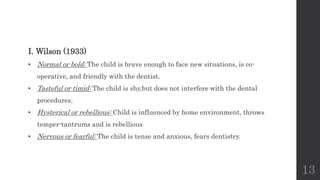
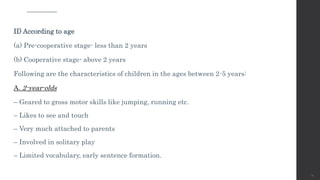
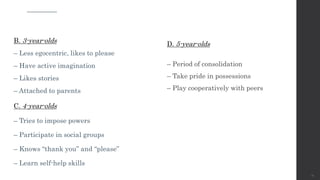
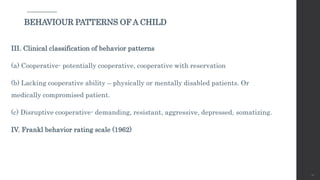
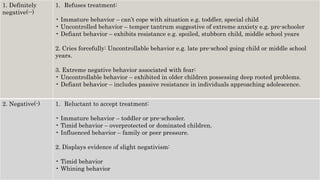
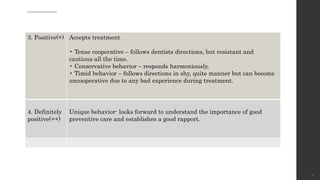
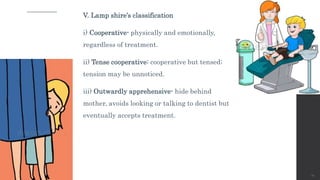
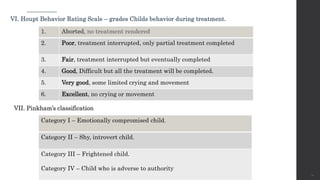
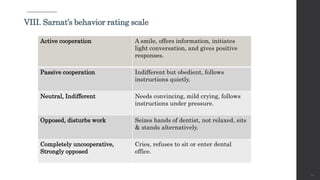
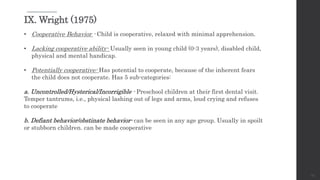
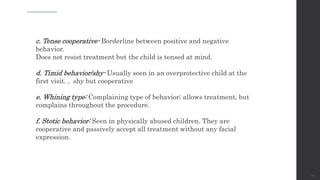
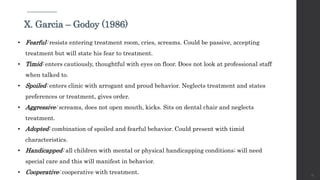
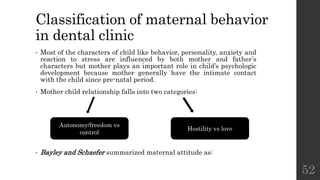
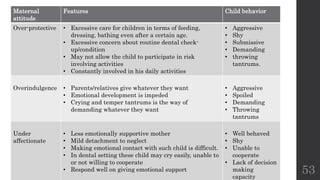
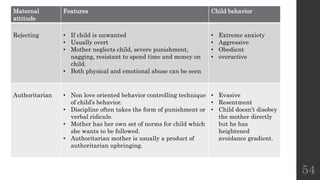
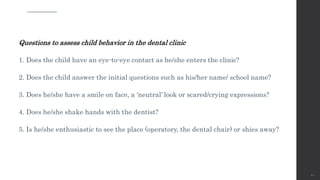
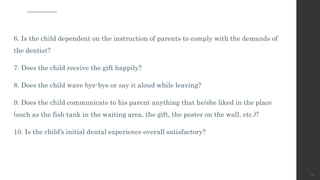
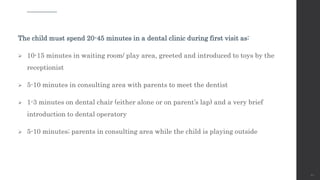
2) Classifications of children's behavior observed in dental clinics according to factors like age and various rating scales.
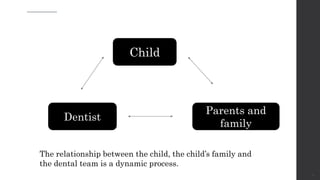
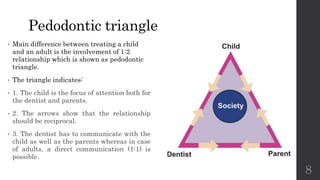
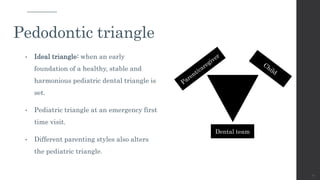
3) Major factors that can affect a child's reaction to dental treatment, including their relationship with parents and dental staff.