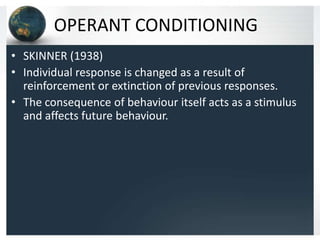
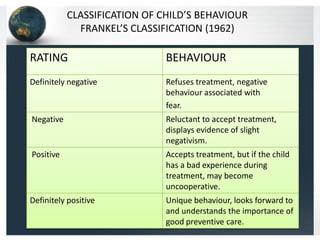
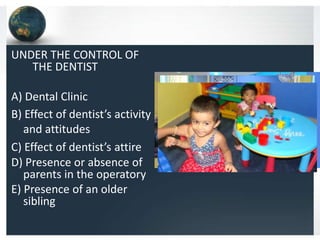
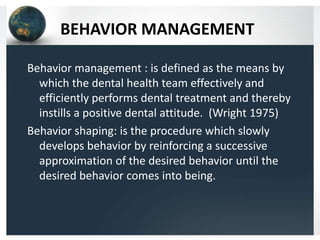
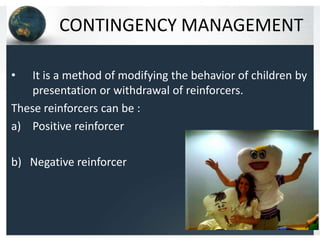
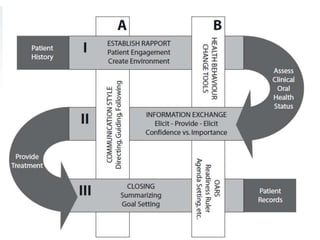
This document summarizes behavioral science concepts related to patient motivation in dentistry. It discusses behavioral theories like classical conditioning, operant conditioning, and social learning theory. It then examines patient behaviors and motivations at different life stages - children, adolescents, adults, and geriatric patients. For each group, factors affecting their behavior are explored along with techniques for behavior management, communication, and motivation. These include psychological approaches like desensitization and modeling as well as pharmacological methods. The goal is to effectively perform treatment while instilling positive dental attitudes.