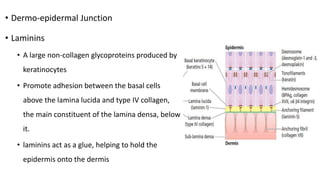
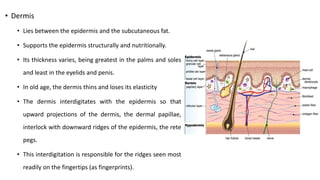
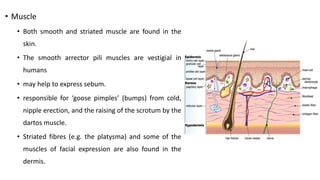
The document summarizes the structure and function of the integumentary system. It describes the skin as having three main layers - the epidermis, dermis and subcutaneous tissue. The epidermis is made of stratified squamous epithelium in multiple layers that acts as a barrier. The dermis lies below and contains collagen, elastic and muscle fibers that provide structure and strength. It also houses hair follicles, sweat glands and nerves. The subcutaneous tissue is made of fat and connective tissue that insulates and cushions the body.