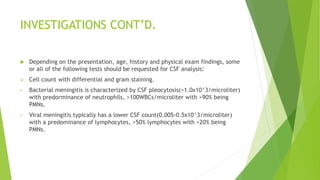
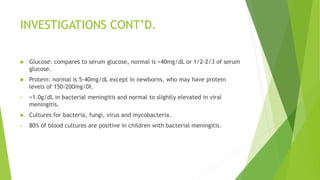
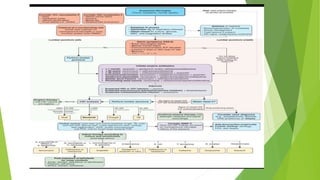
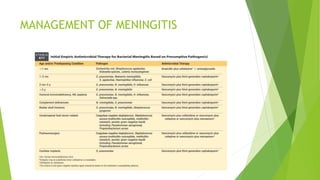
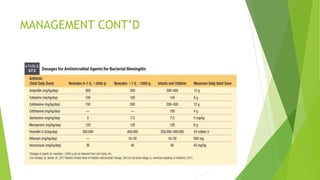
The document discusses meningitis in pediatrics, covering its definition, etiology, modes of transmission, pathophysiology, clinical presentation, investigation methods, and management strategies. It highlights key causes of meningitis, including bacterial, viral, and fungal origins, along with risk factors and potential complications such as hearing loss and increased intracranial pressure. The document serves as a comprehensive overview for understanding meningitis and its impact on pediatric health.