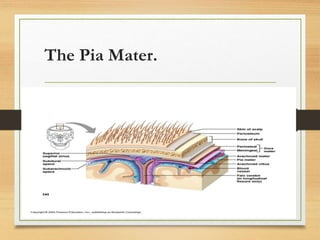
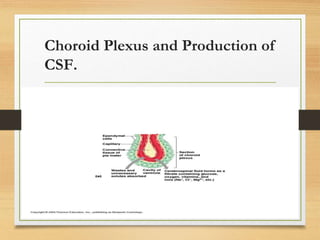
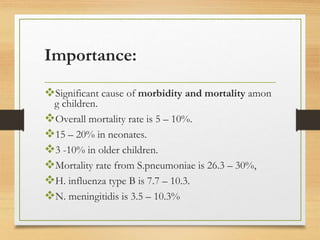
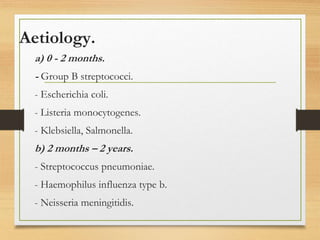
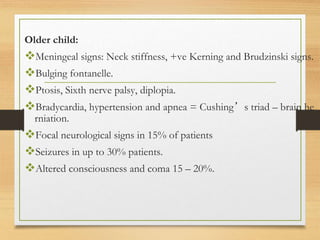
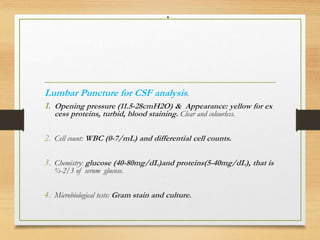
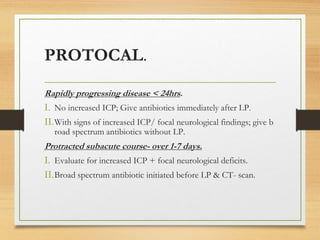
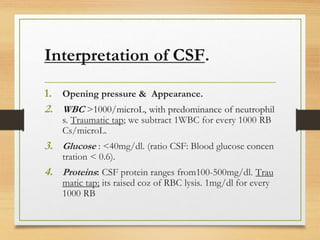
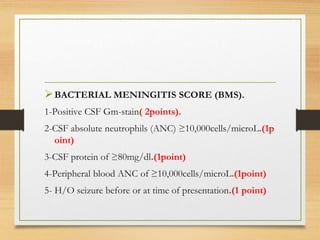
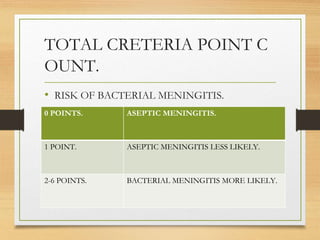
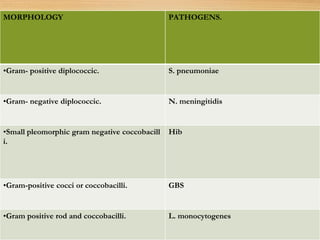
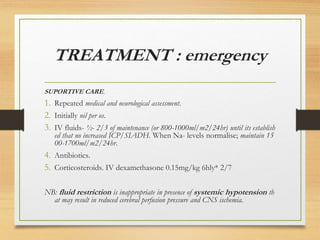
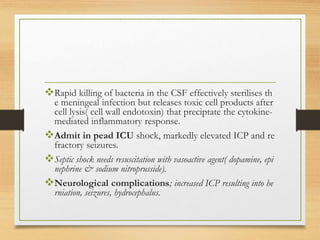
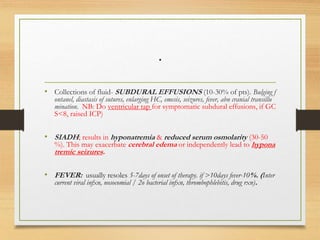
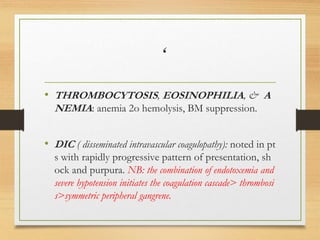
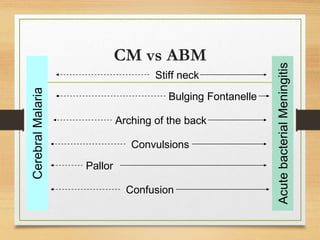
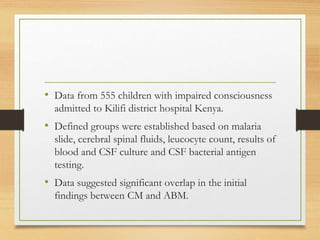
This document provides information on acute central nervous system infections, including bacterial meningitis and cerebral malaria. It defines meningitis as inflammation of the two inner layers of tissue covering the brain and spinal cord. It describes the relevant anatomy of the brain and meninges. Common causes of bacterial meningitis are discussed for different age groups. Risk factors, pathogenesis, clinical features, differential diagnosis, and initial investigations for meningitis and cerebral malaria are summarized. Lumbar puncture indications, contraindications, and analysis of cerebrospinal fluid are also outlined.