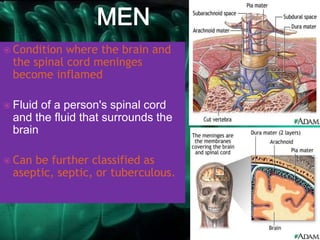
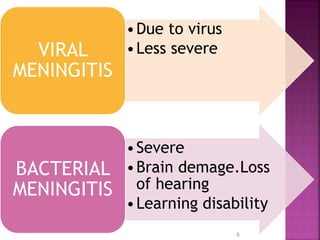
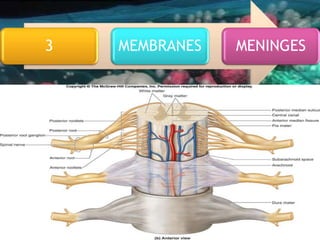
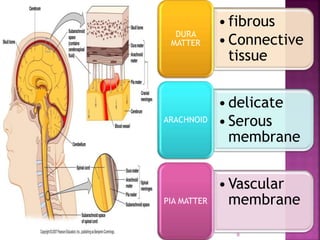
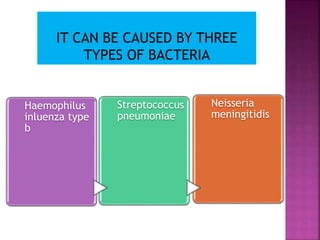
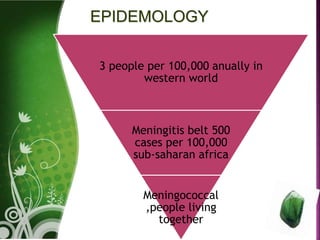
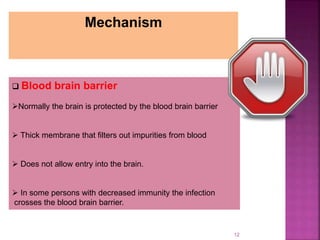
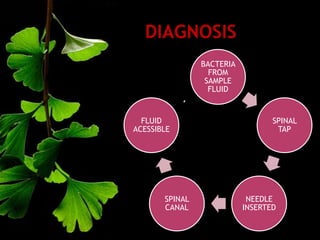
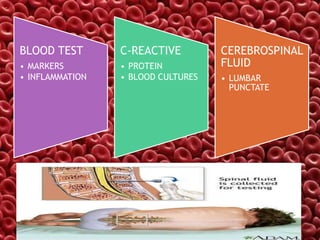
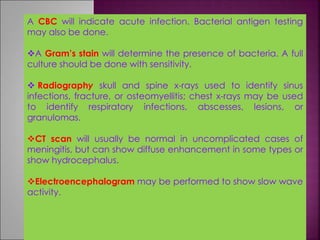
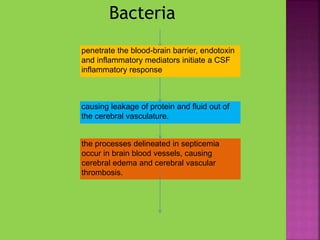
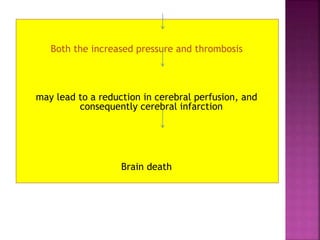
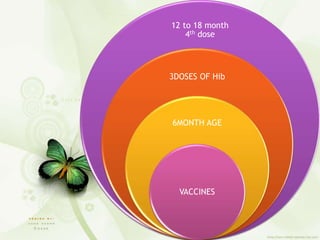
This document discusses meningitis, an inflammation of the meninges that surround the brain and spinal cord. It can be caused by viruses or bacteria entering the blood and crossing the blood-brain barrier. Common symptoms include fever, headache, and neck stiffness. Diagnosis involves spinal taps, blood tests, and scans. Treatment is with antibiotics and supportive care. Vaccines can help prevent some forms of bacterial meningitis.