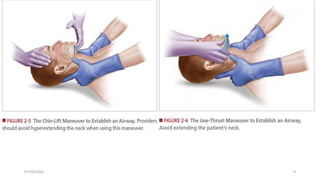
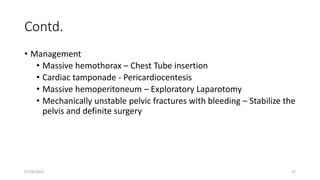
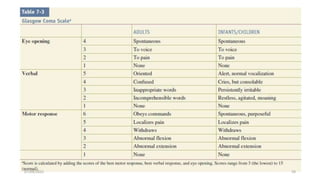
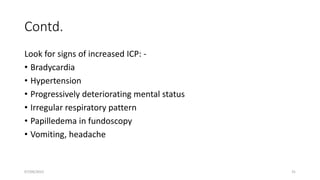
This document provides an overview of the Advanced Trauma Life Support (ATLS) protocol for managing trauma patients in the emergency room. It discusses the primary, secondary, and tertiary surveys used to systematically evaluate trauma patients and identify life-threatening injuries. The primary survey focuses on the ABCDEs - airway, breathing, circulation, disability, and exposure. The secondary survey involves a full physical exam and history. Adjunct tests help identify specific injuries. The tertiary survey re-examines patients within 24 hours to find any missed injuries, as up to 13% of injuries are initially overlooked.