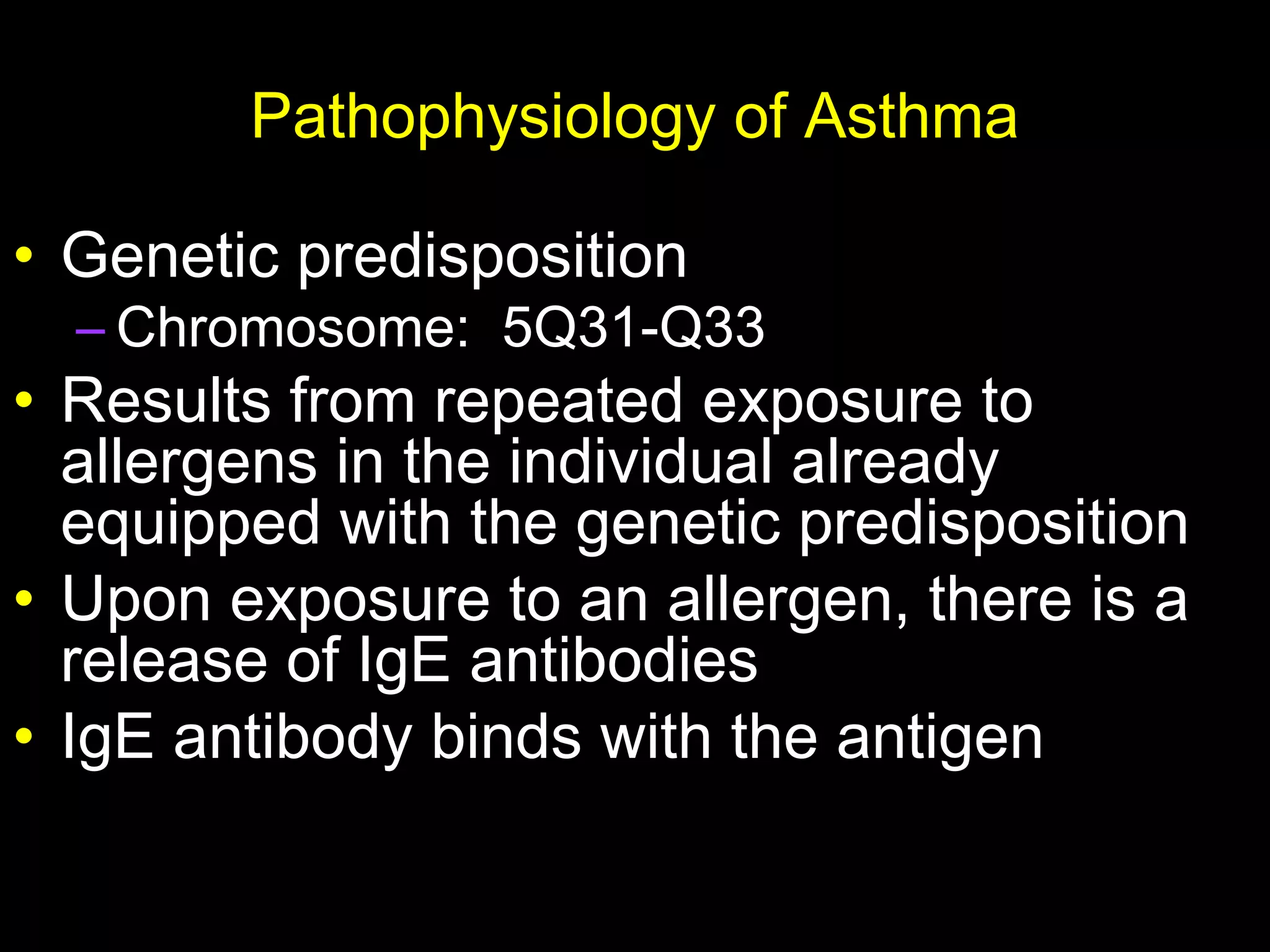
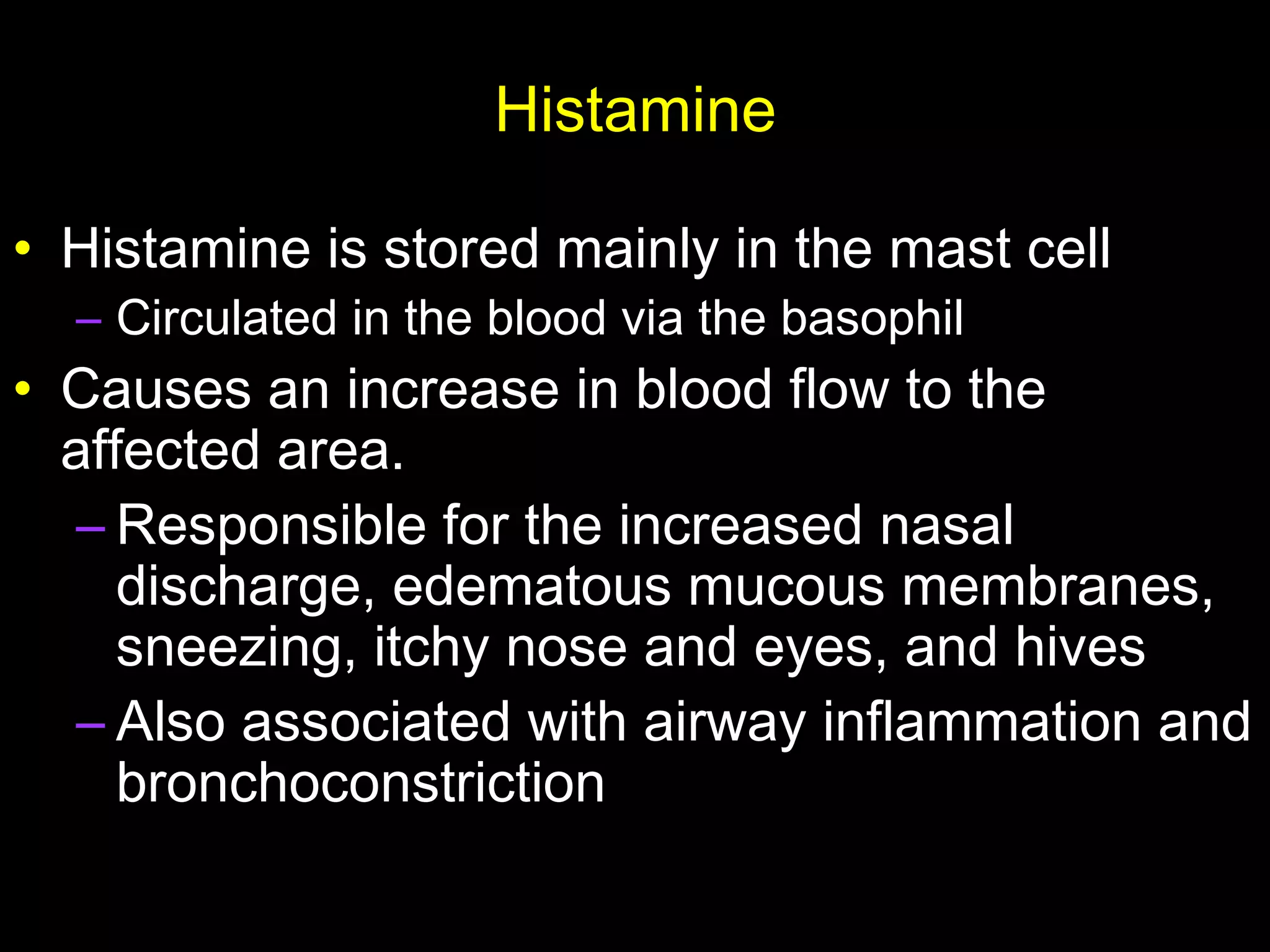
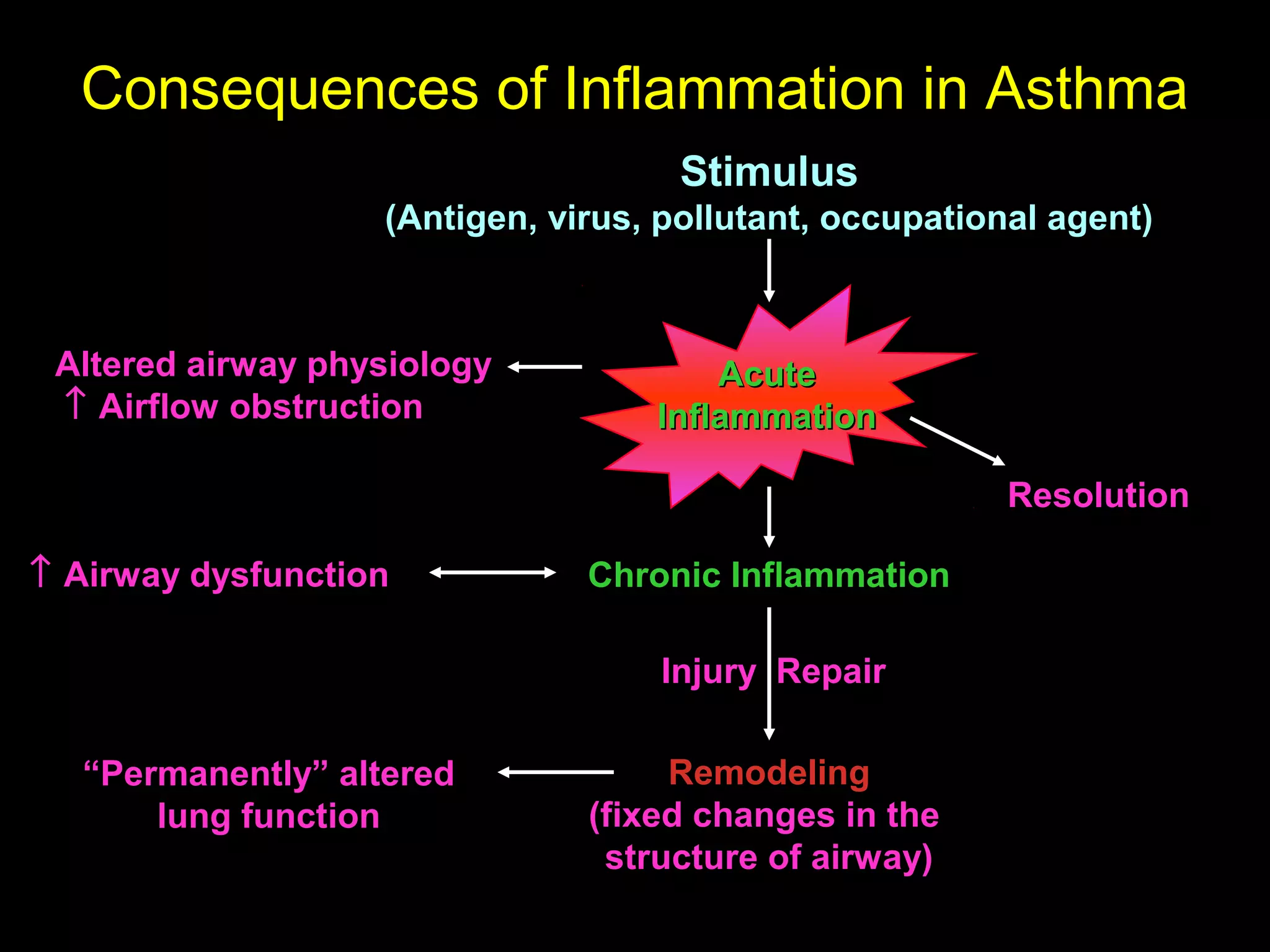
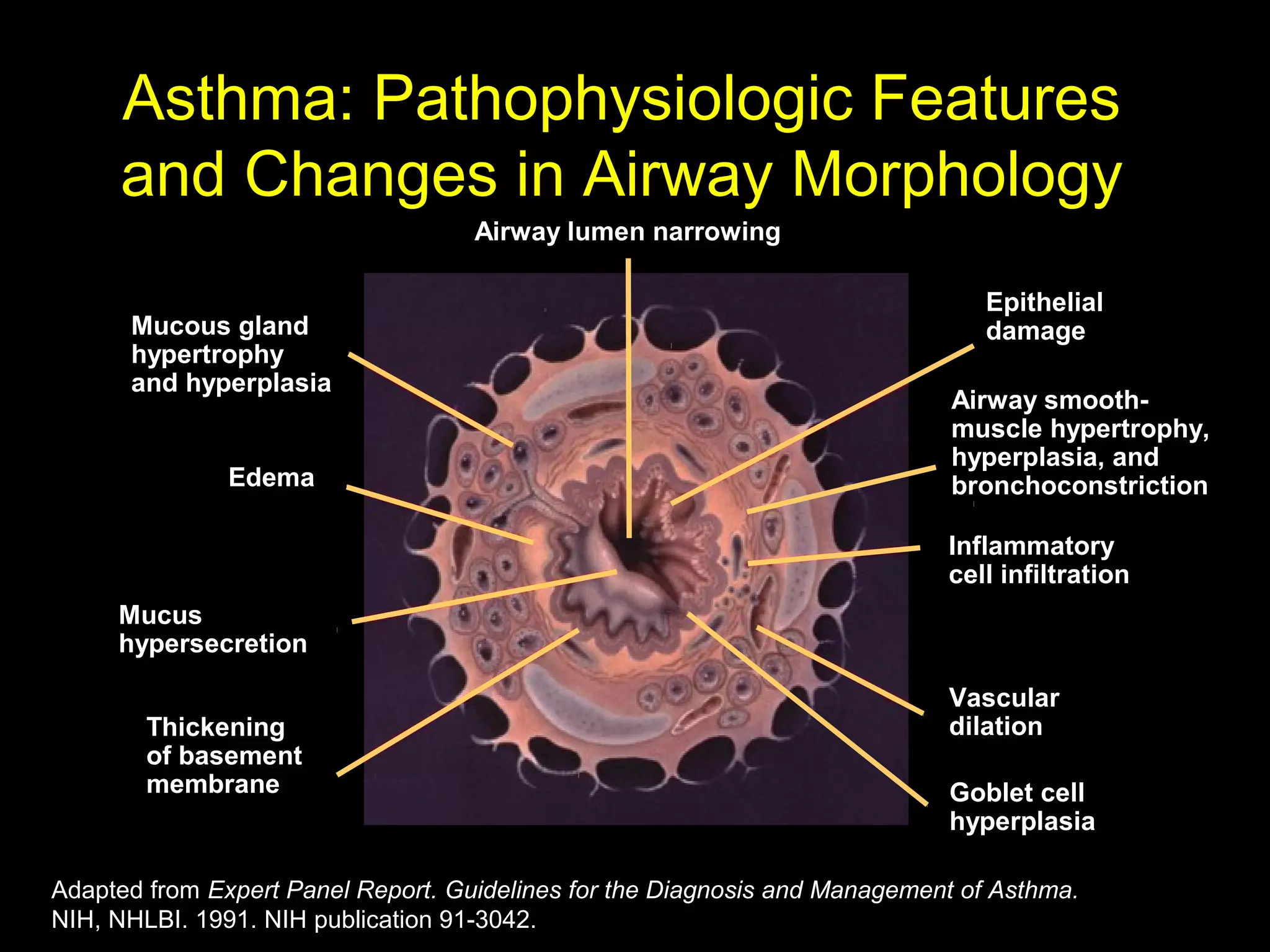
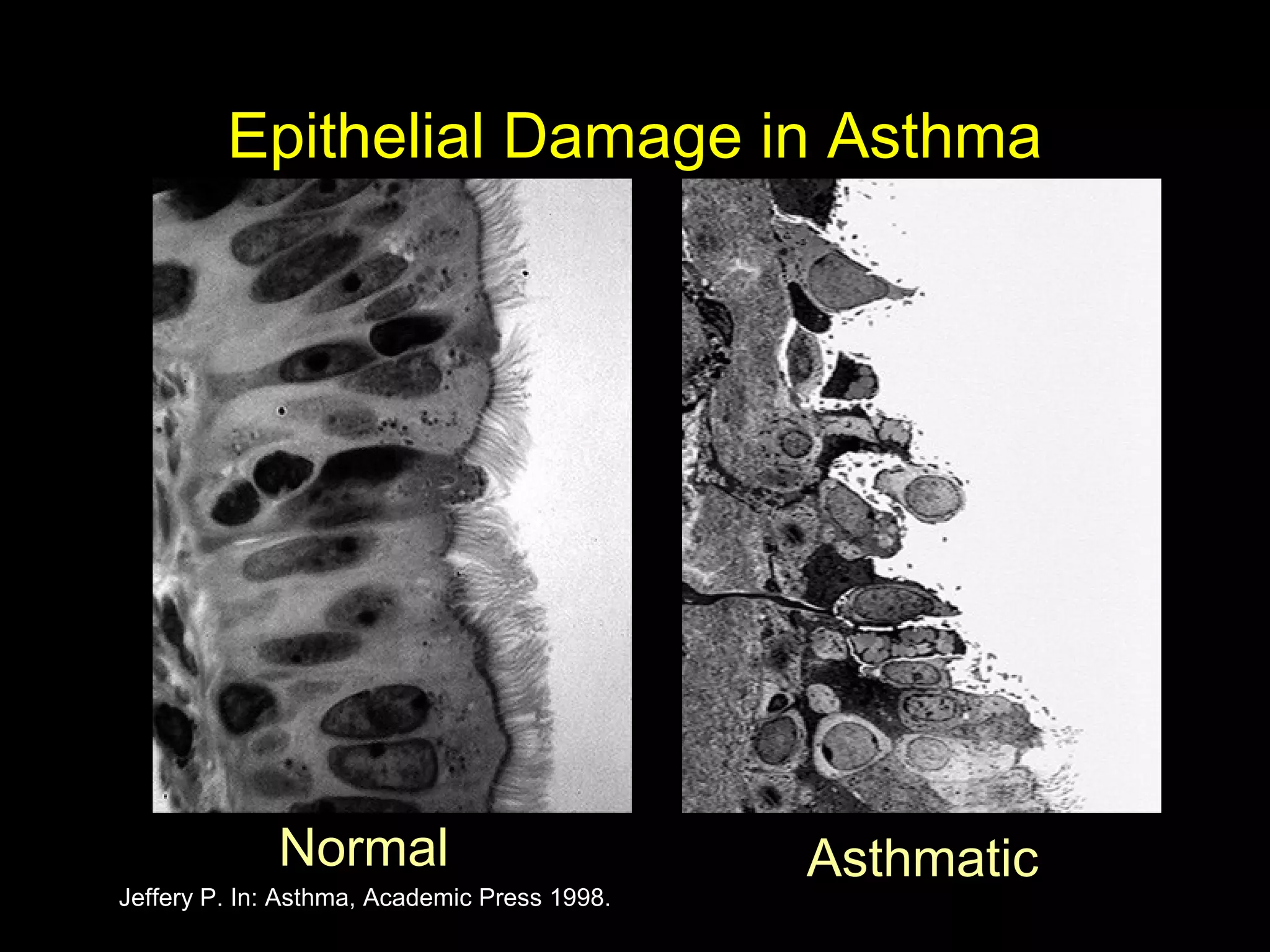
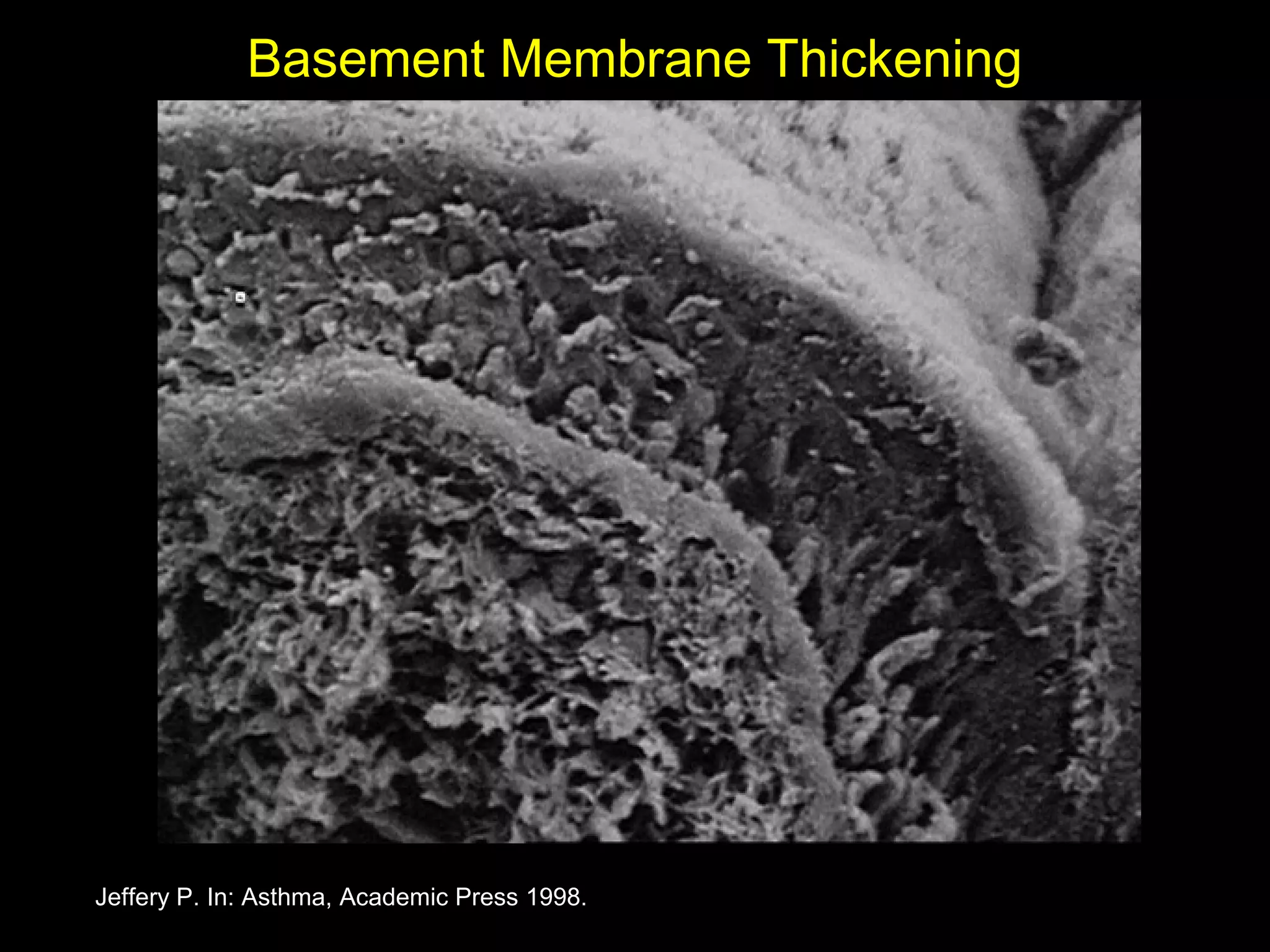
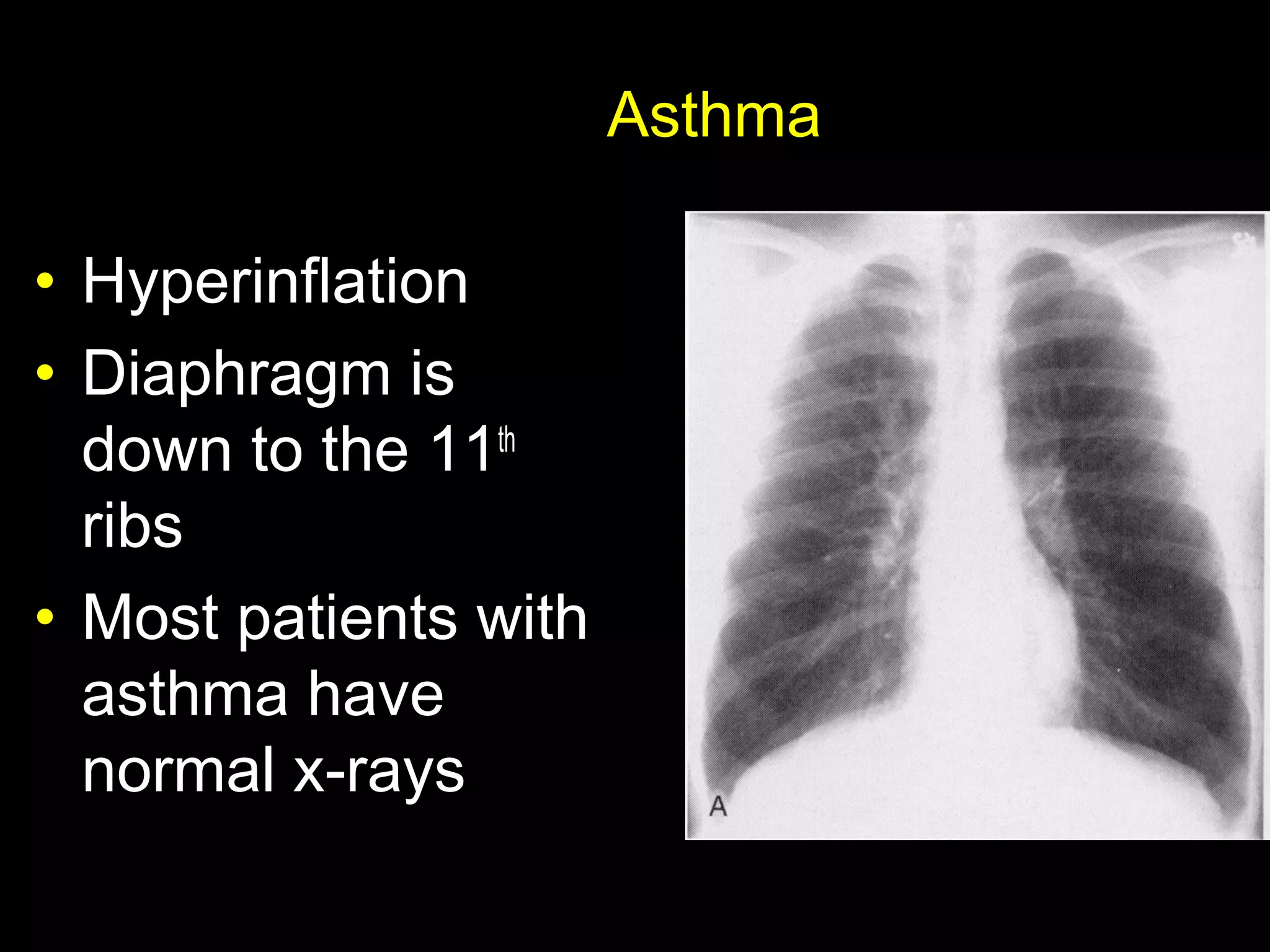
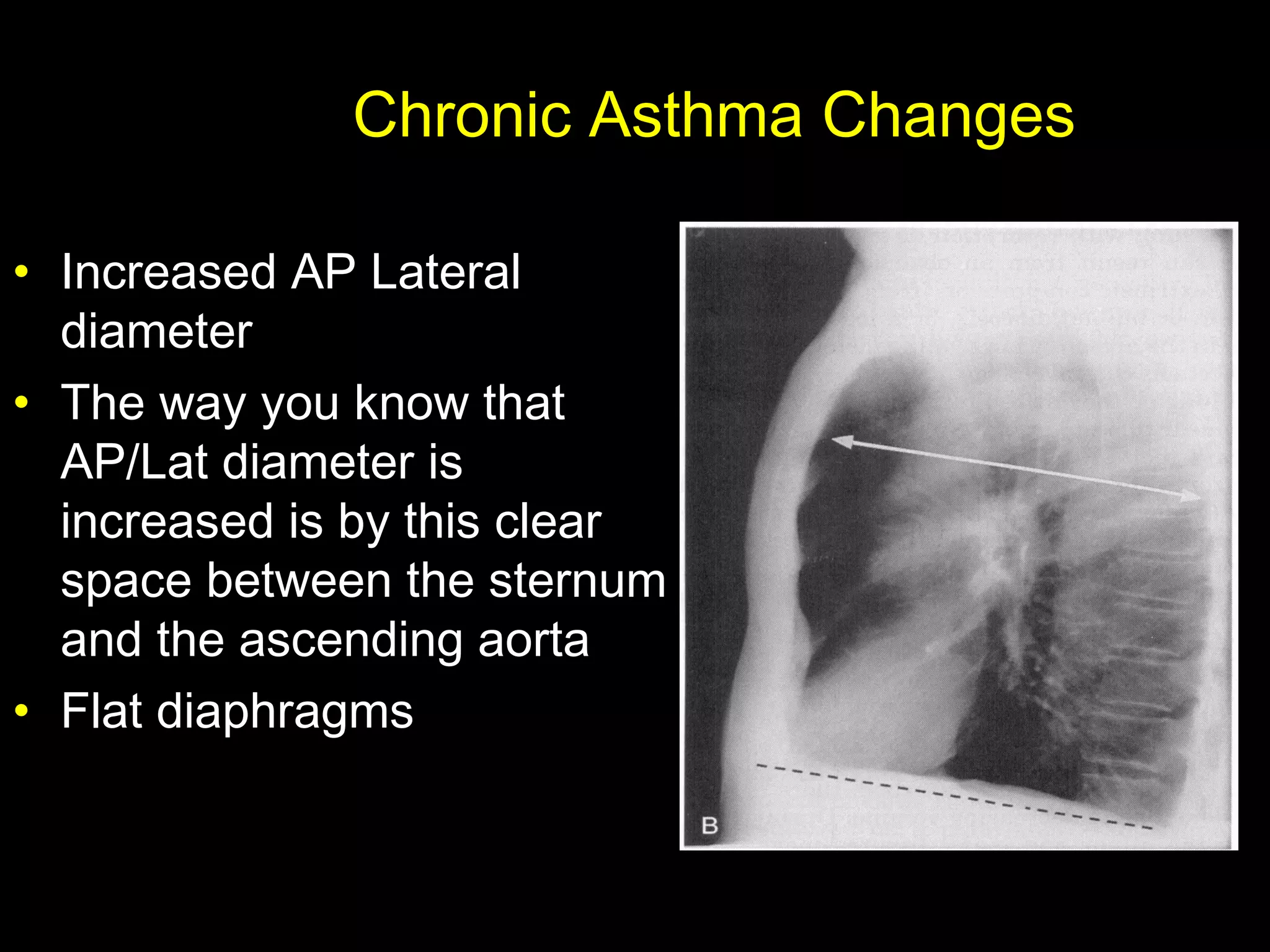
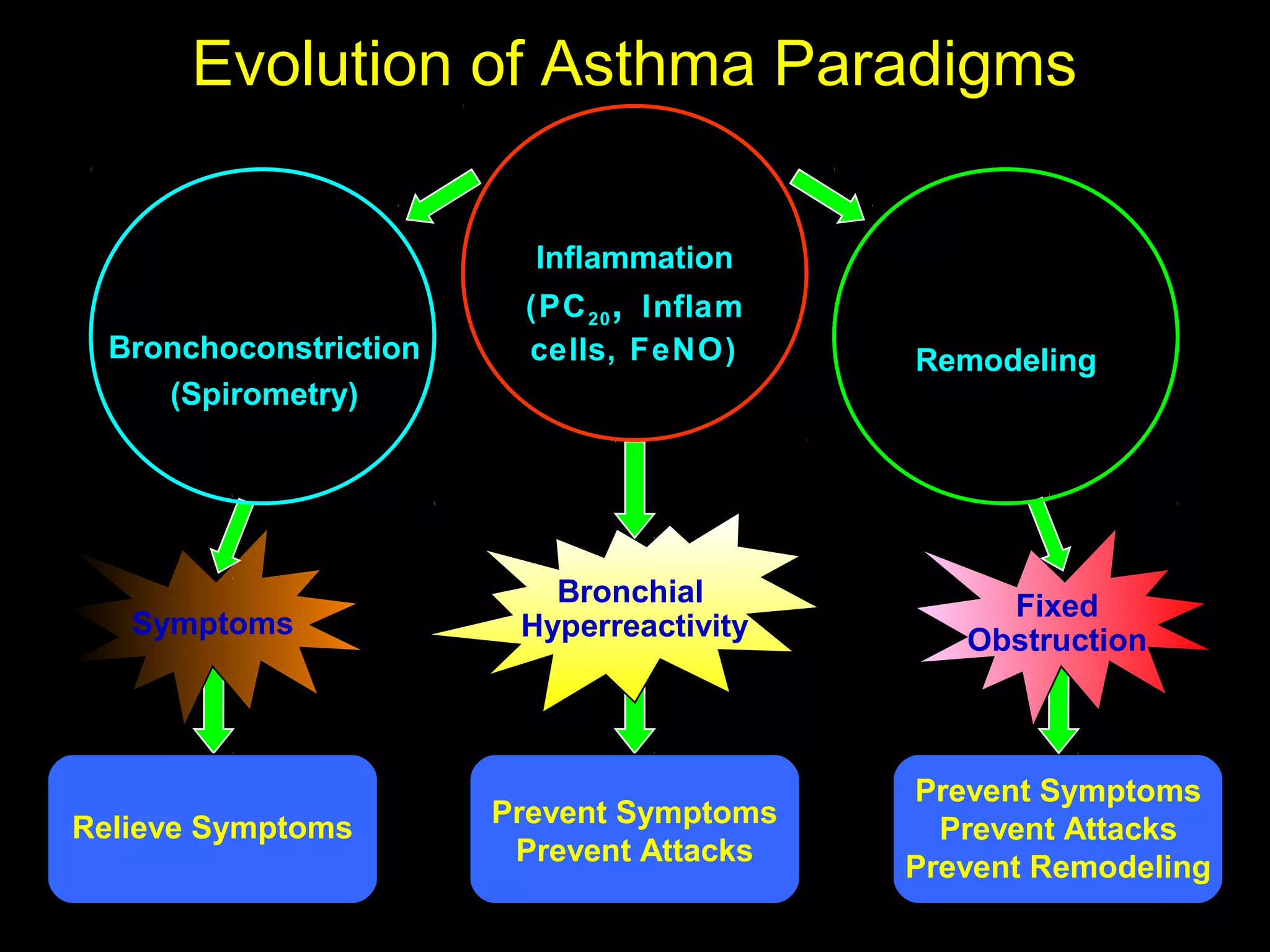
- Asthma is a chronic lung disease characterized by airway inflammation and narrowing of the airways. It causes symptoms like wheezing, coughing, and shortness of breath.
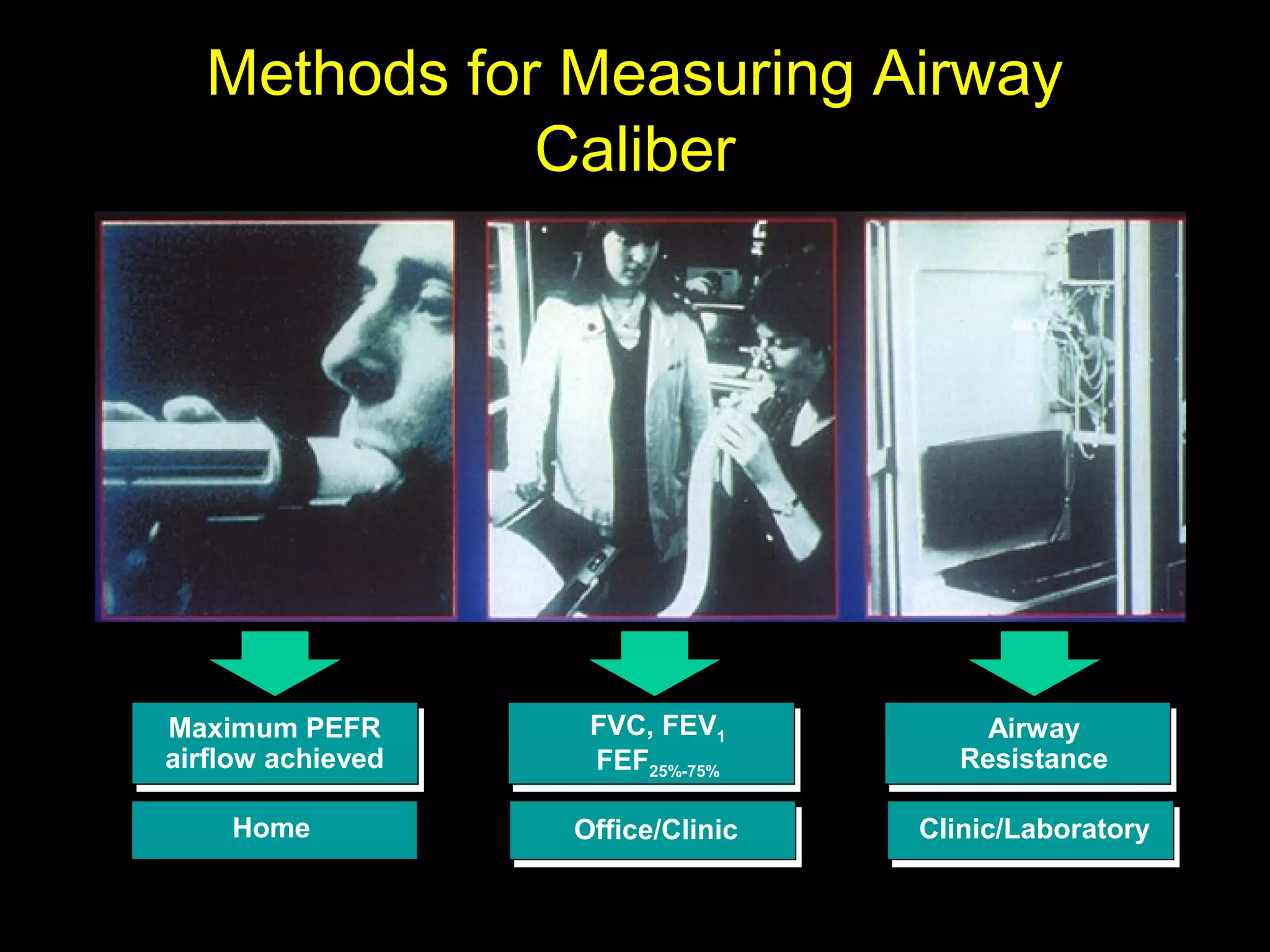
- It is diagnosed based on a patient's medical history and symptoms, and confirmed via spirometry testing which shows improved lung function after use of a bronchodilator.
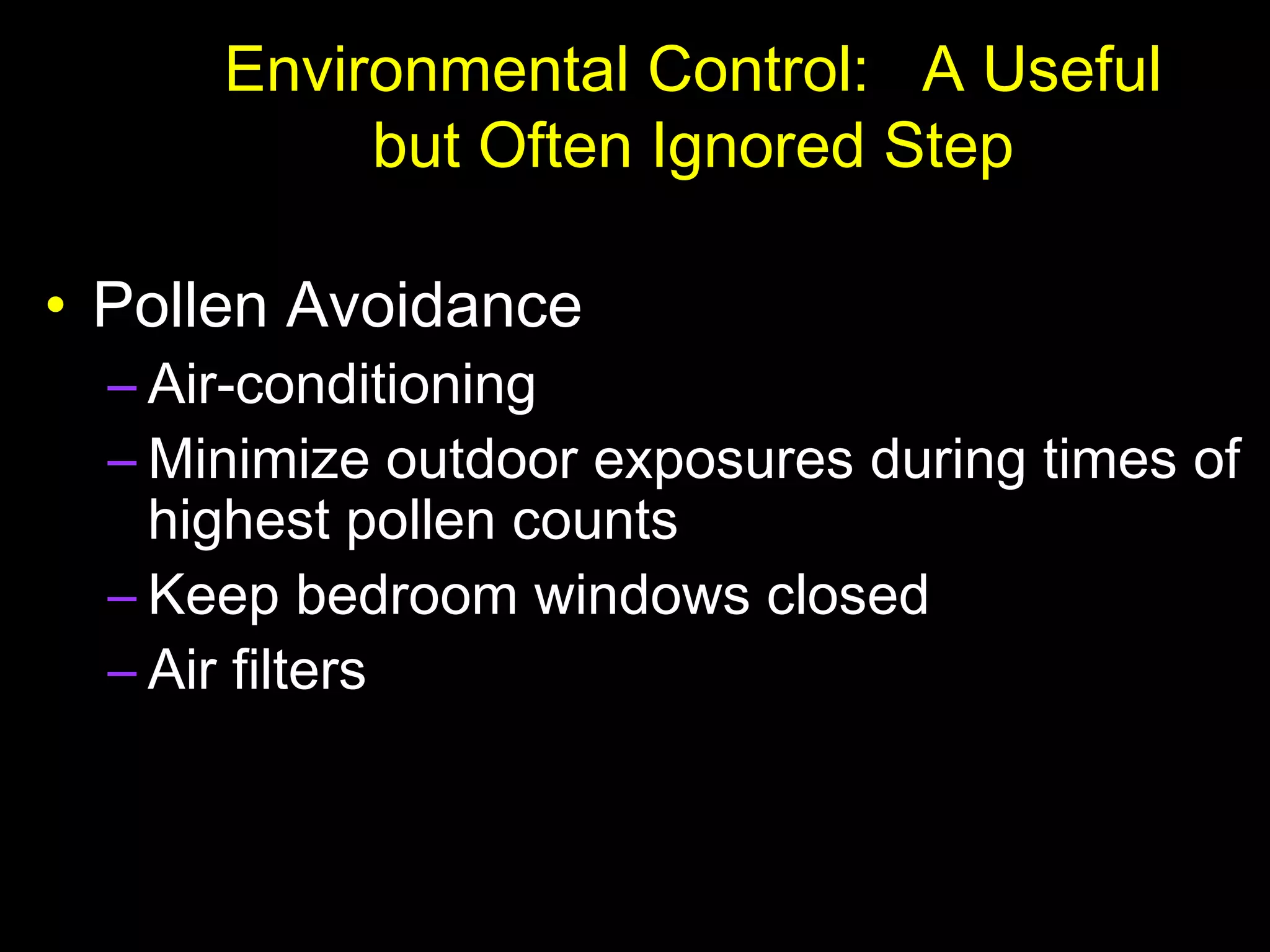
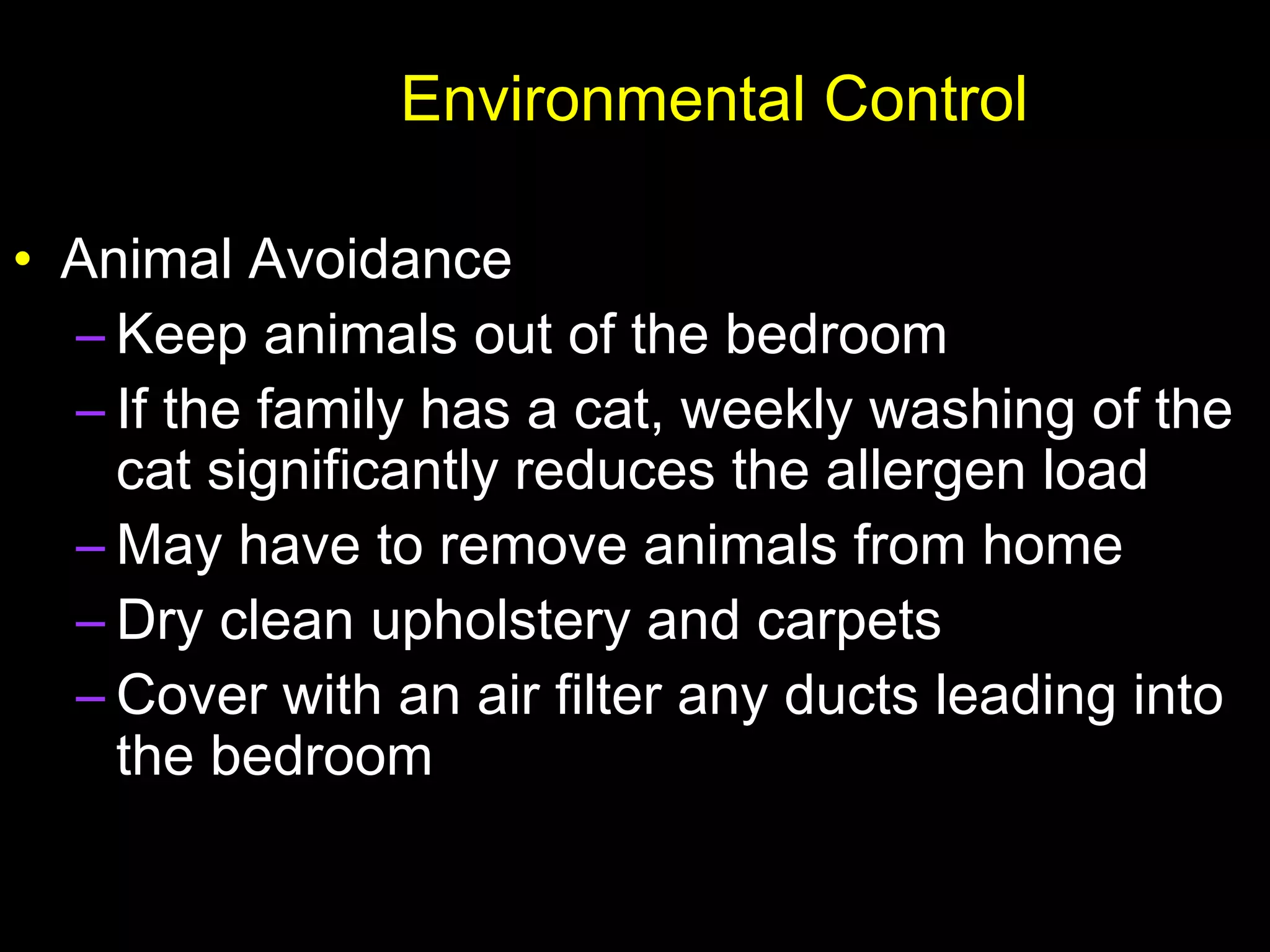
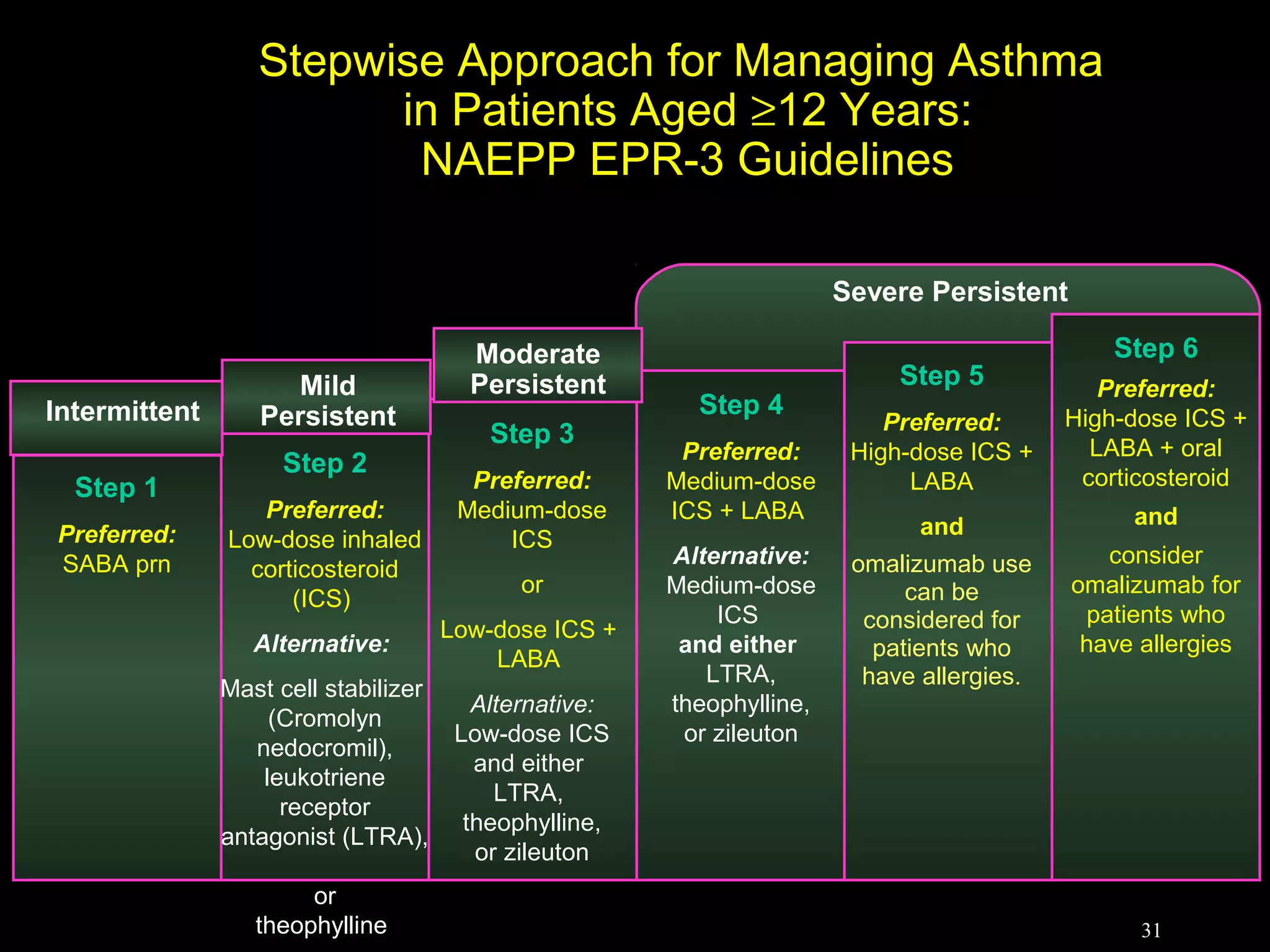
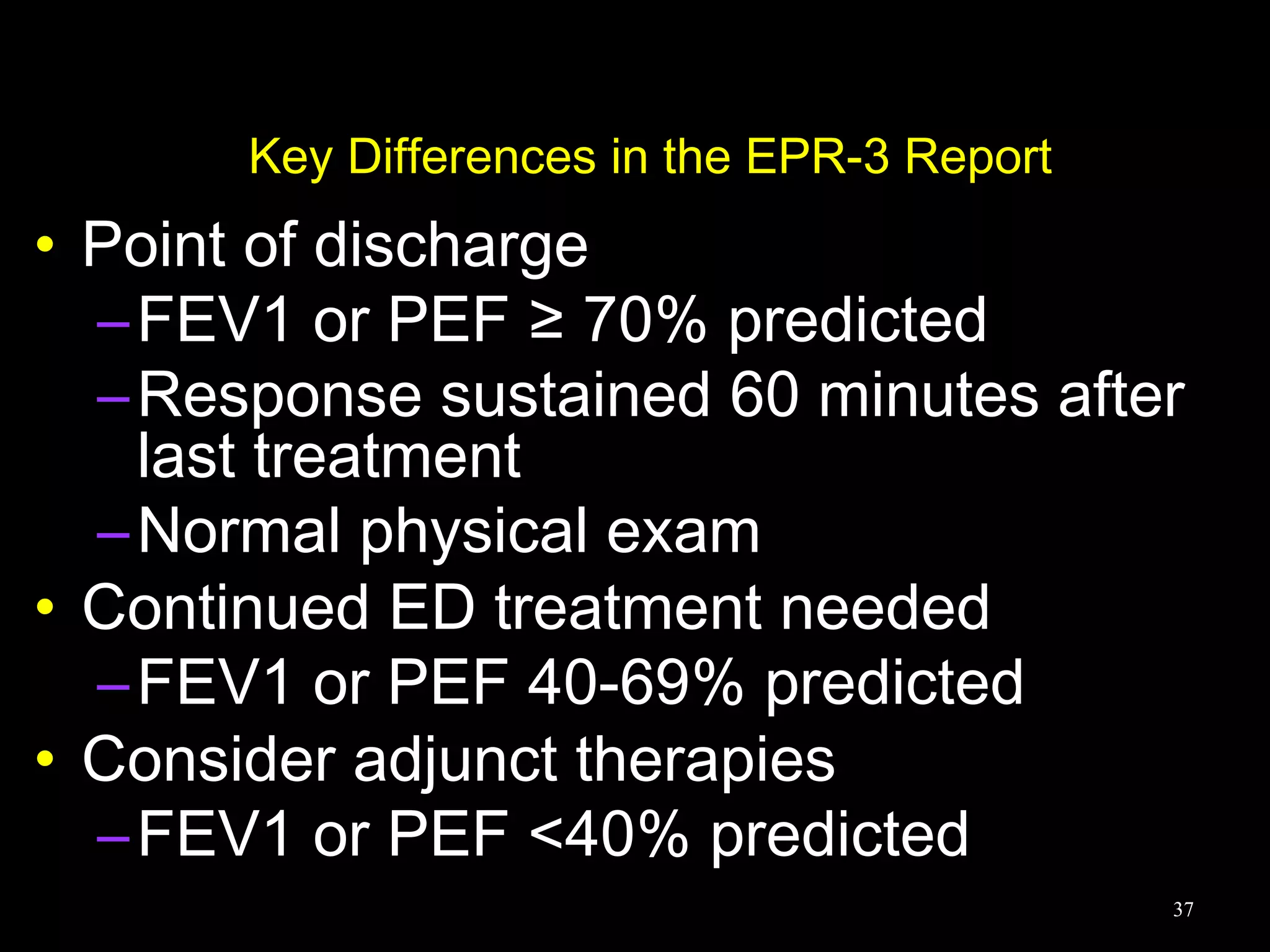
- Treatment involves controlling triggers, medications like inhaled corticosteroids to reduce inflammation, and managing exacerbations which involve increasing medications under a treatment plan.