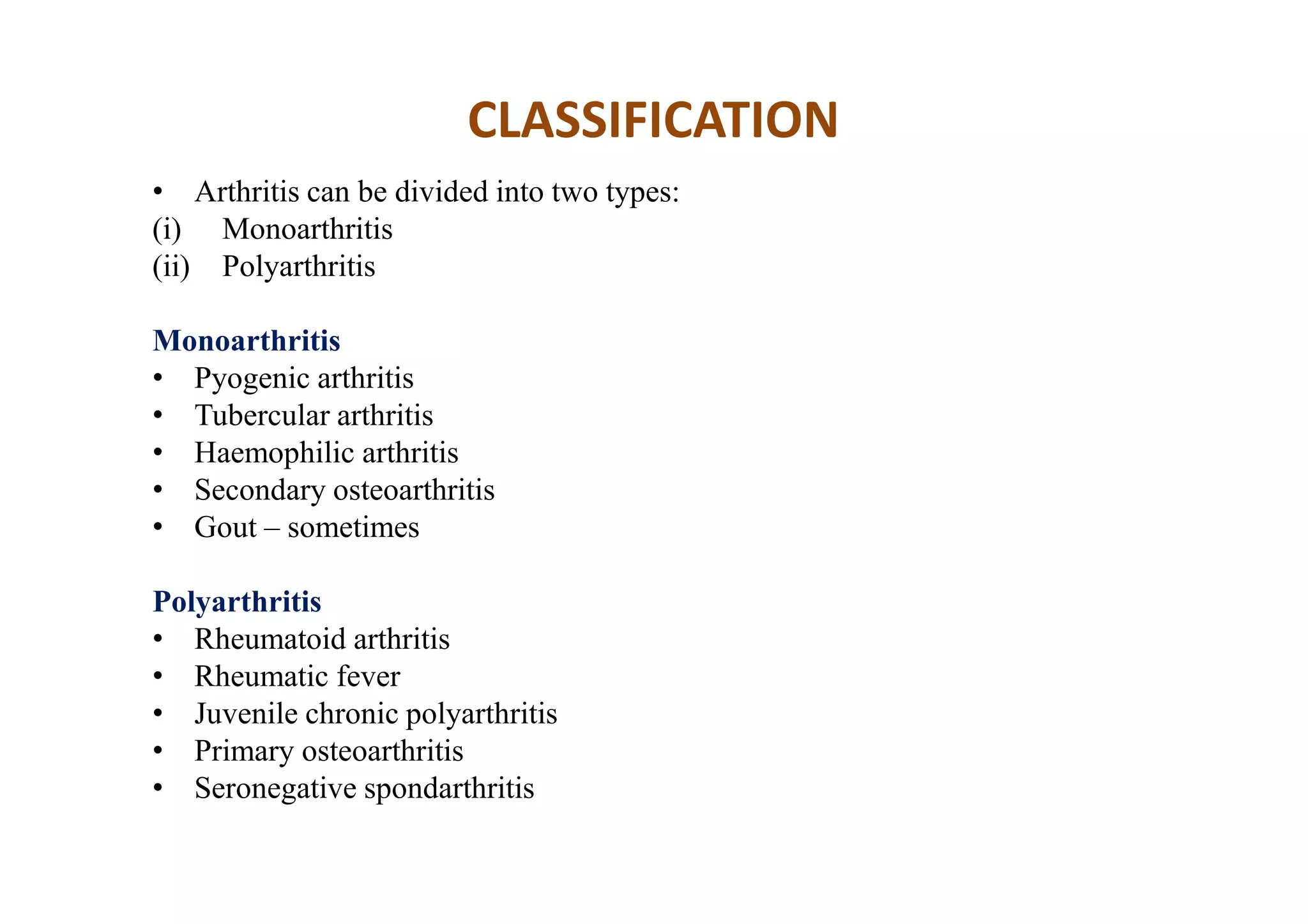
This document discusses arthritis and related diseases. It defines arthritis as inflammation of a joint and describes its main causes and types. Rheumatoid arthritis is discussed in detail, including its pathology, clinical features, diagnostic criteria, and treatments. Ankylosing spondylitis and osteoarthritis are also summarized. The document provides overviews of the classifications, presentations, investigations, and management approaches for different forms of arthritis.