This document provides an overview of arthritis, including:
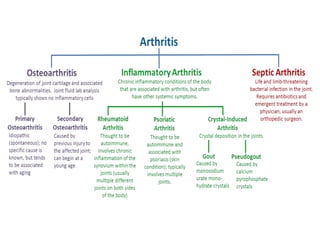
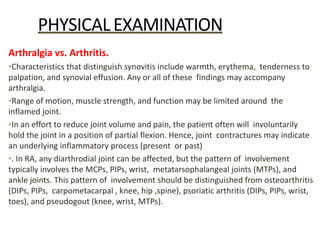
- Definitions of true arthritis versus periarticular joint pain
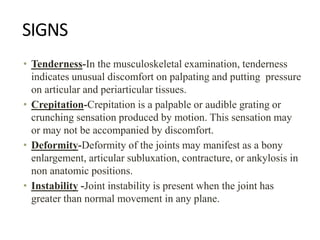
- Common symptoms of arthritis like pain, swelling, stiffness, limitation of motion
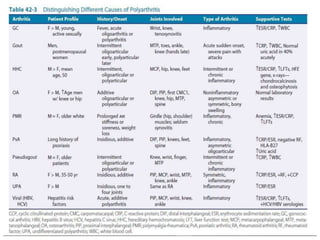
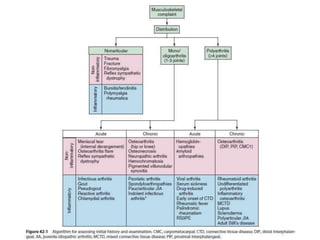
- Classification of arthritis based on number of joints involved and duration
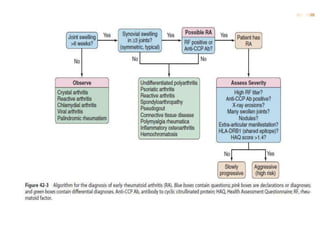
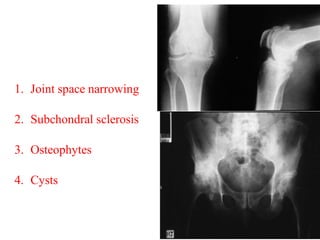
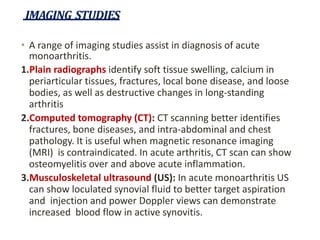
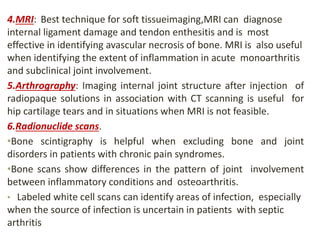
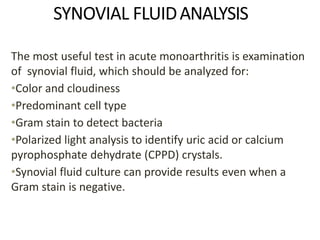
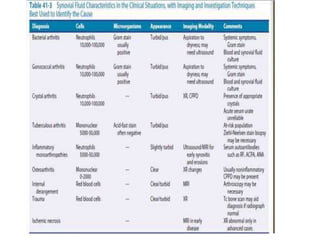
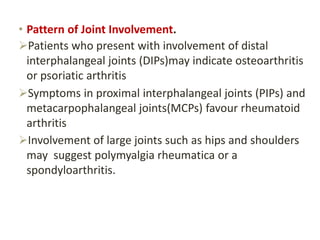
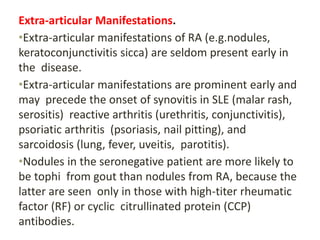
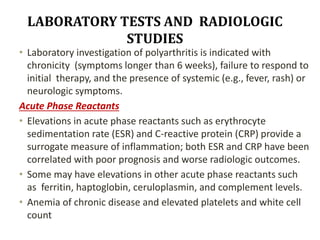
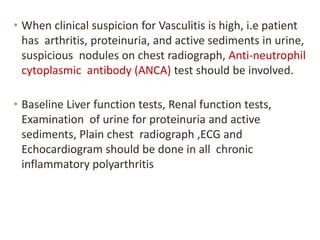
- Approaches to evaluating monoarthritis and polyarthritis through history, exam, labs, imaging
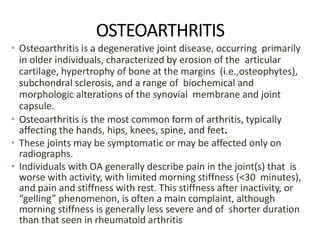
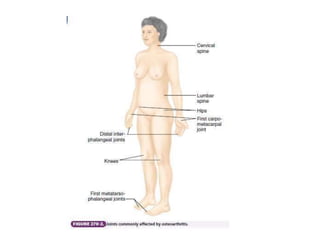
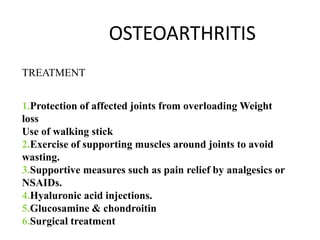
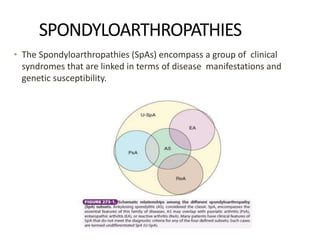
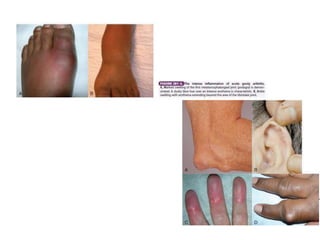
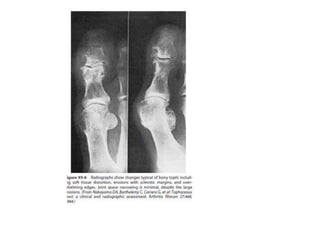
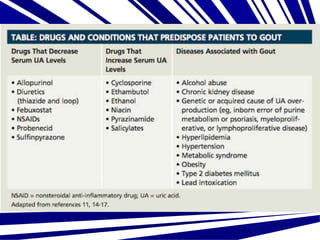
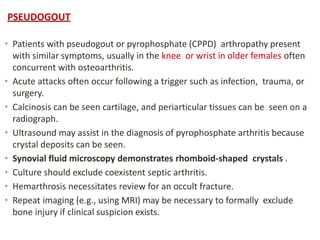
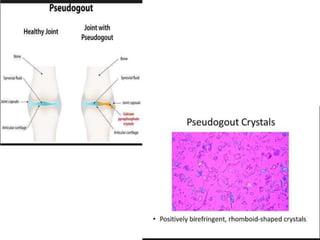
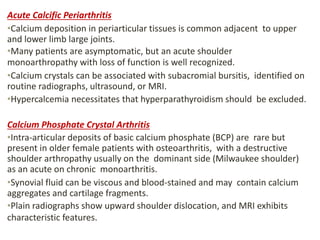
- Details on specific types of arthritis like gout, pseudogout, osteoarthritis

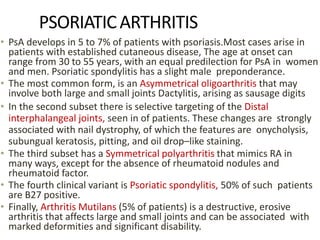
![APPROACH TOPOLYARTHRITIS
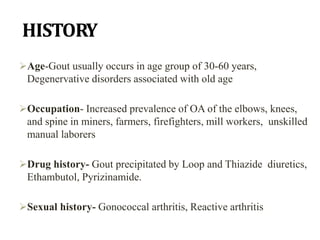
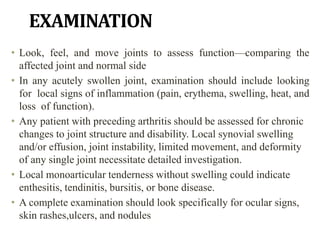
1)HISTORY:
•Demographics. Age, sex, and family background may
provide clues to the type of arthritis. Gout is more
common in men ; osteoarthritis affects older patients
more often than younger counterparts, and in
spondyloarthritides familial association
•Symptom Onset. If patients present with abrupt onset
of symptoms, consider infection, gout, pseudogout, or
trauma, whereas if symptoms were present for
months/years, rheumatoid arthritis (RA), psoriatic
arthritis (PsA), chronic infection (e.g., syphilis, hepatitis,
human immunodeficiency virus [HIV]) and OA are
differentials.](https://image.slidesharecdn.com/arthritis-221108083333-6df4cea1/85/Arthritis-pptx-32-320.jpg)

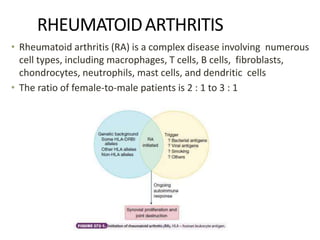
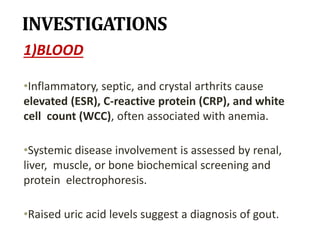
![Serologies
• Serum rheumatoid factor (RF),autoantibody (typically
immunoglobulin [Ig]M) that binds to the Fc component of IgG
and may play a role in acute inflammatory arthritis.
• Approximately 20% of patients meeting American College of
Rheumatology(ACR) classification criteria for RA are seronegative.
• The presence of the RF has been found to be predictive of
persistent disease and progression with radiologic damage in
patients with inflammatory arthritis.
• Other serologic markers that have been evaluated for use in early
diagnosis of RA include the Anticitrullinated protein antibodies
(ACPAs or CCP Ab), which are nearly as sensitive as RF but are far
more specific for RA.
• If the CCP Ab test is combined with the RF, one can expect a
sensitivity of 58% with a specificity of 100%; positive and
negative predictive values are 100% and 88%, respectively.](https://image.slidesharecdn.com/arthritis-221108083333-6df4cea1/85/Arthritis-pptx-40-320.jpg)