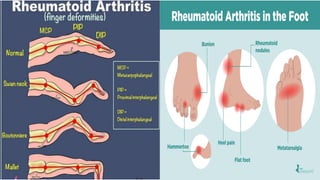
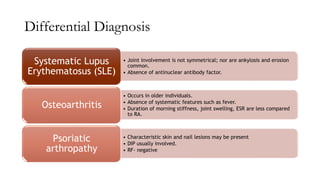
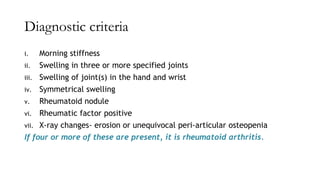
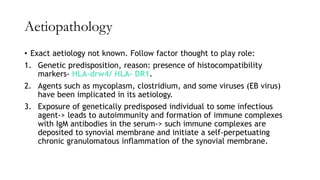
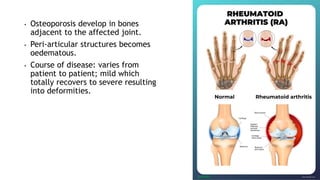
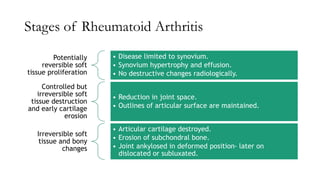
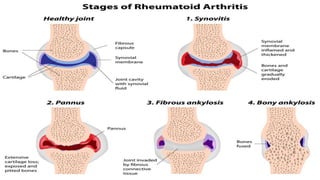
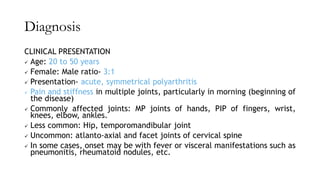
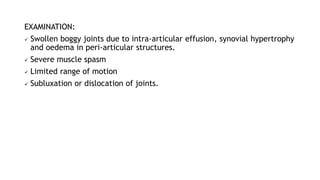
The document provides an overview of rheumatoid arthritis, including its classification, diagnostic criteria, aetiopathology, stages, and treatment options. It emphasizes the chronic nature of the condition, symptoms like morning stiffness and joint swelling, and outlines the progression from reversible soft tissue changes to irreversible damage. Treatment focuses on medication, physiotherapy, and potential surgical interventions aimed at preserving joint function and preventing deformities.

![INVESTIGATIONS
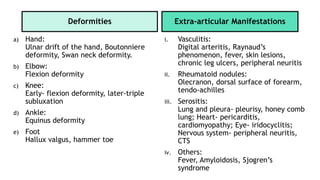
I. Radiological examination: consist of X-rays of affected joints. Findings:
Reduced joint space
Erosion of articular cysts
Subchondral cysts
Juxta-articular rarefaction
Soft tissue shadow at the level of joint (joint effusion or synovial
hypertrophy)
Deformities of hand and fingers
II. Blood:
Elevated ESR
Low haemoglobin value
Rheumatoid factor- auto antibody directed against Fc fragment of
immunoglobulin G (IgG) [Can be checked via Latex fixation test or Rose-
Waaler test]
Note: all the patients with RF do not have RA and vice versa
III. Synovial fluid examination
IV. Synovial biopsy](https://image.slidesharecdn.com/ra-230731182001-c38f6239/85/Rheumatoid-Arthritis-pdf-15-320.jpg)