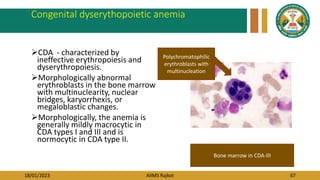
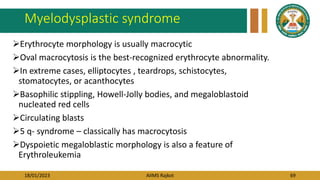
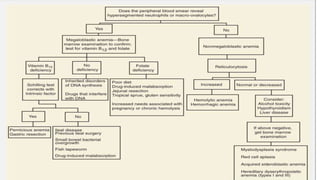
This document provides an overview of macrocytic anemia, including:
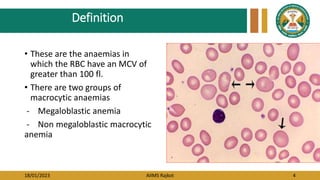
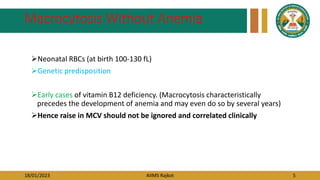
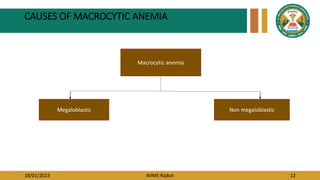
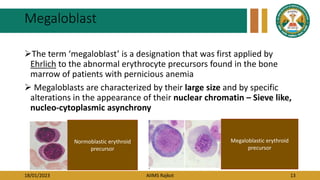
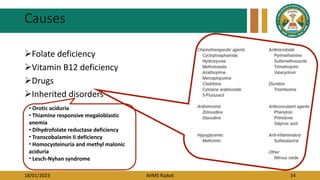
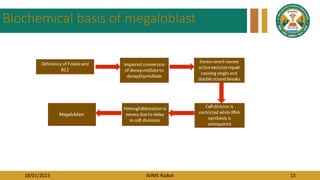
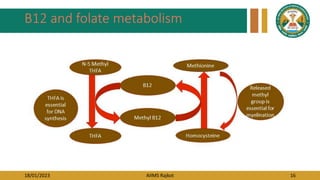
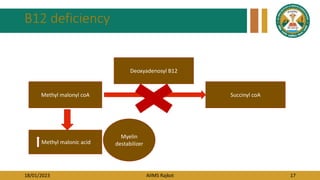
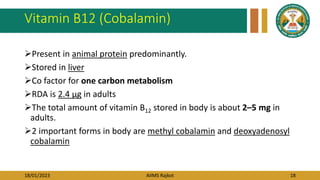
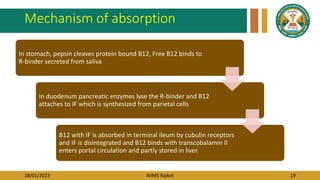
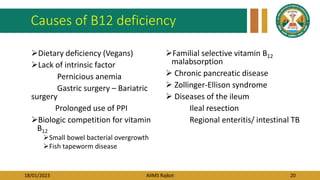
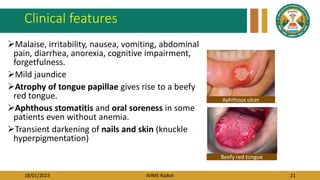
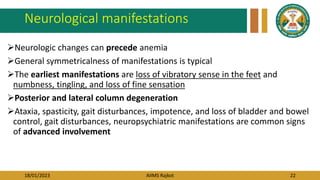
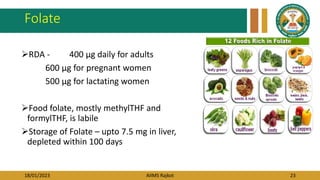
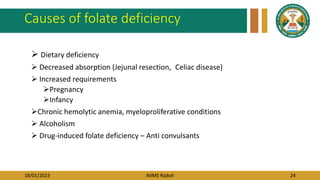
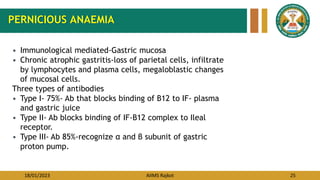
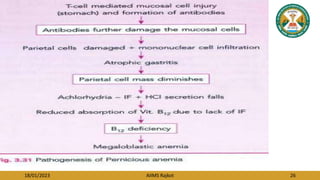
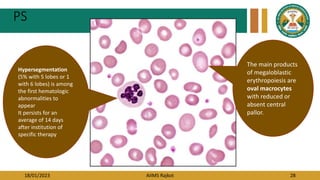
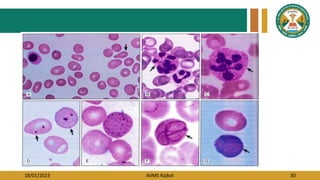
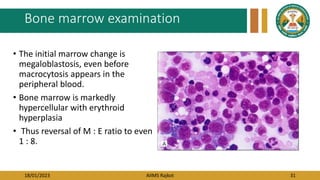
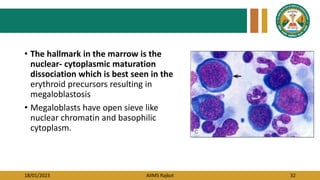
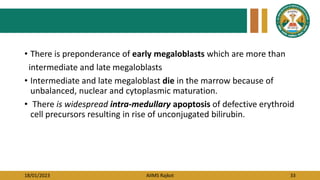
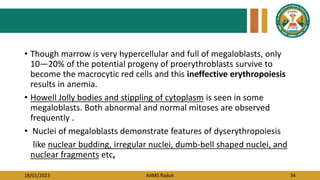
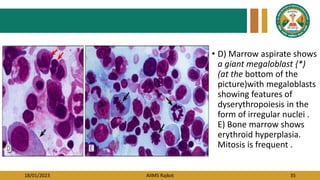
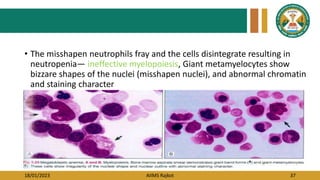
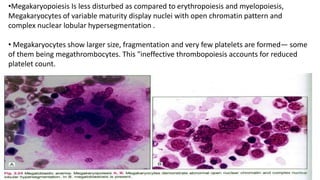
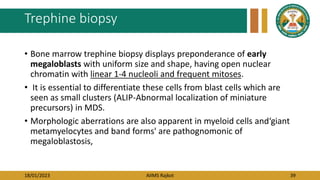
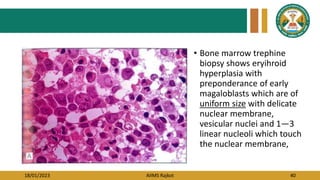
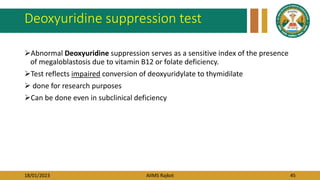
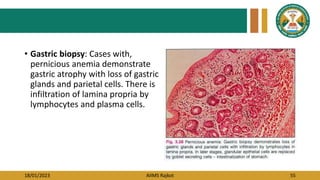
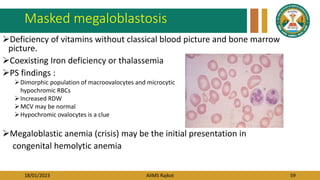
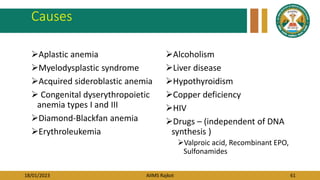
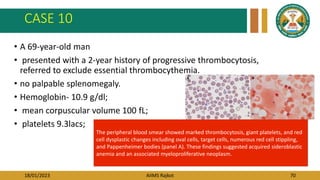
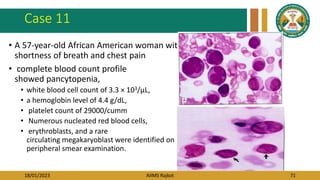
- Megaloblastic anemia is caused by vitamin B12 or folate deficiency and results in large, immature red blood cells (megaloblasts) in the bone marrow.
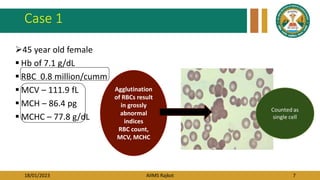
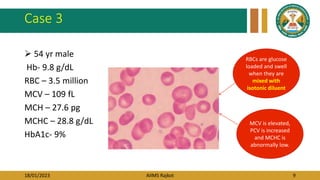
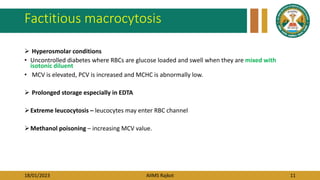
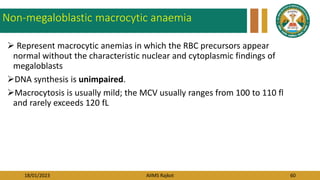
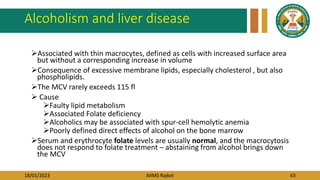
- Non-megaloblastic macrocytic anemias have other causes and do not involve megaloblasts.
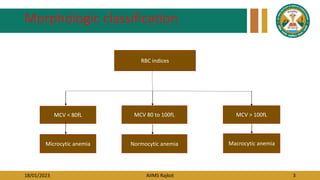
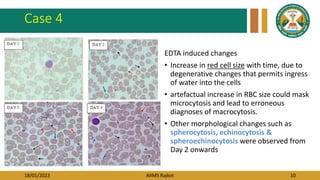
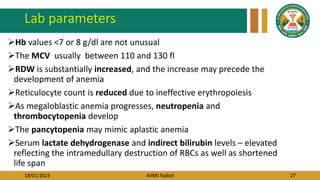
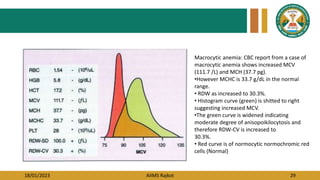
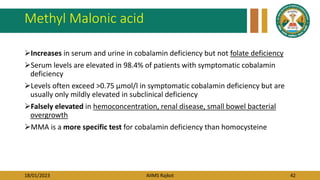
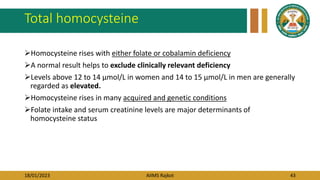
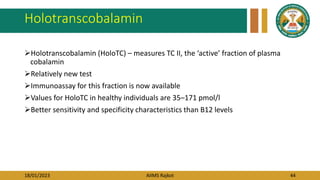
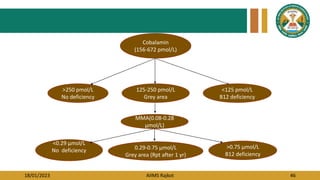
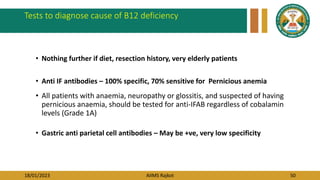
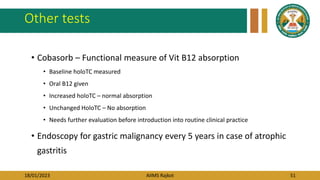
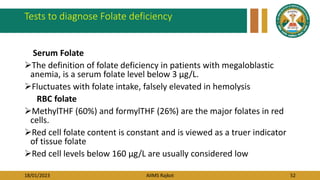
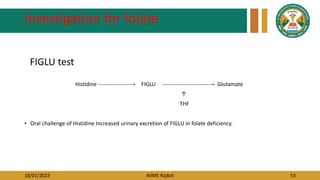
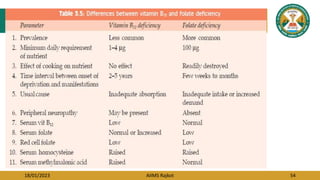
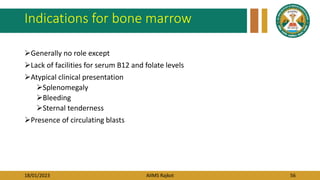
- Workup of macrocytic anemia includes evaluation of mean corpuscular volume, red cell distribution width, blood counts, serum B12 and folate levels, and bone marrow examination showing megaloblasts in megaloblastic anemia.
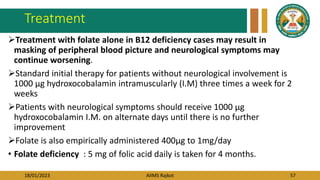
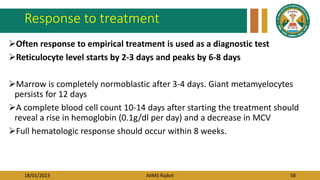
- Treatment depends on the underlying cause but commonly involves B