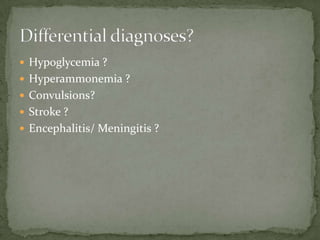
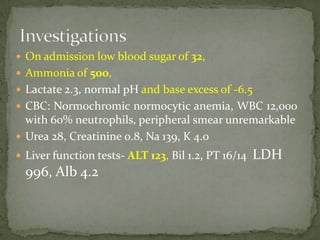
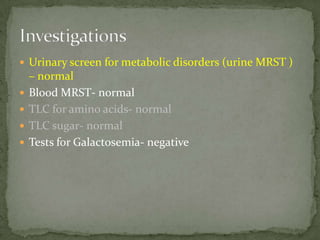
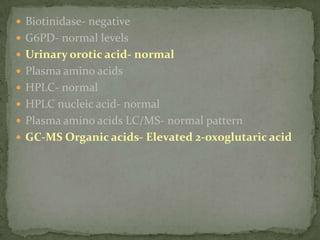
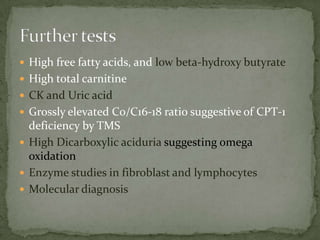
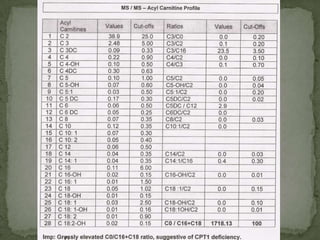
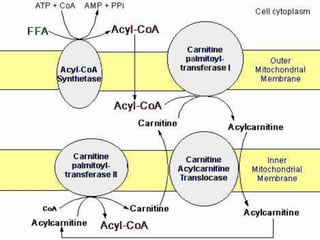
This document describes the case of a 3-year-old boy who presented with recurrent loss of consciousness following trivial illness. Initial workup revealed hypoglycemia and hyperammonemia. Further testing found elevated 2-oxoglutaric acid and a high C0/C16-18 ratio suggestive of carnitine palmitoyltransferase I (CPT-I) deficiency. The patient was diagnosed with a fatty acid oxidation disorder and treated accordingly.