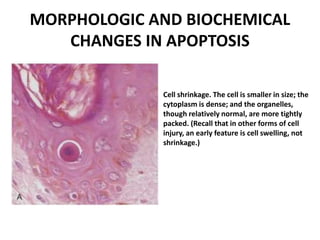
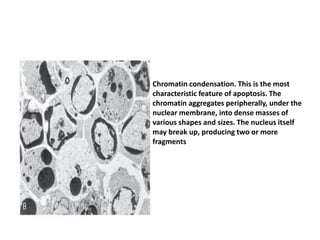
Apoptosis is a tightly regulated process of programmed cell death where cells activate enzymes to degrade their own DNA and proteins. The plasma membrane remains intact but becomes a target for phagocytes. The dead cell and fragments are rapidly consumed before contents can leak out, preventing inflammation. Apoptosis eliminates damaged, unneeded, or harmful cells and occurs during development, tissue remodeling, and to limit damage from infections or DNA damage. It is characterized by cell shrinkage, chromatin condensation, and fragmentation into membrane-bound apoptotic bodies.