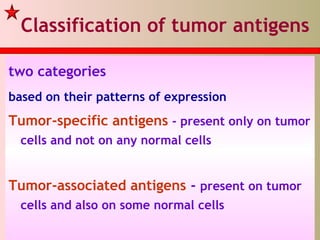
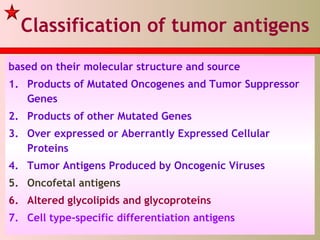
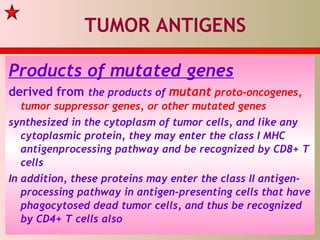
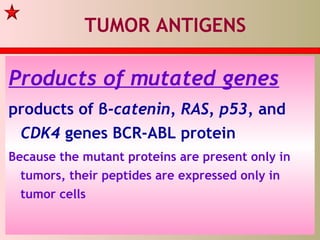
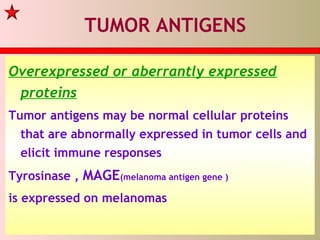
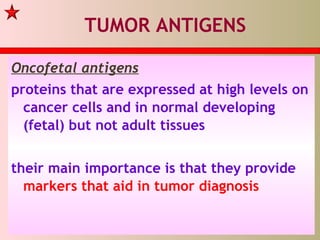
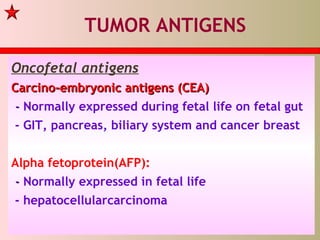
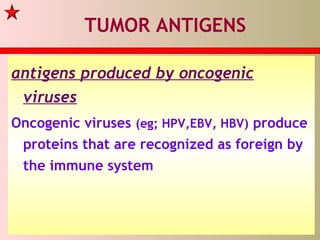
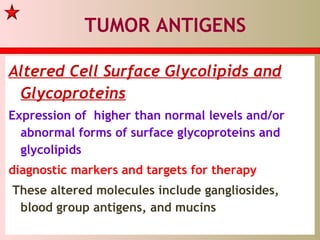
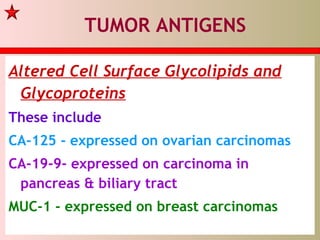
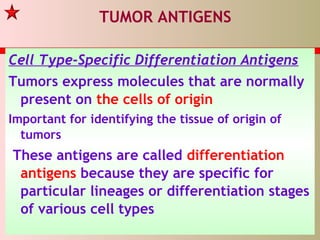
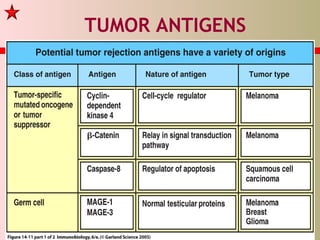
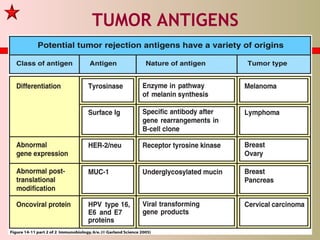
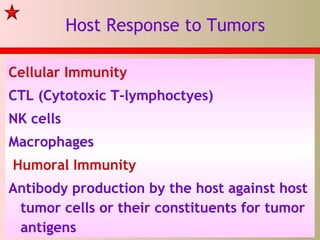
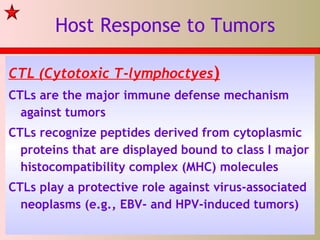
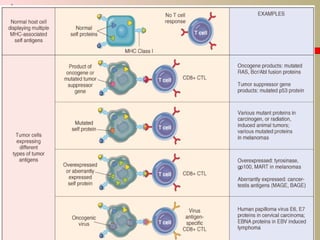
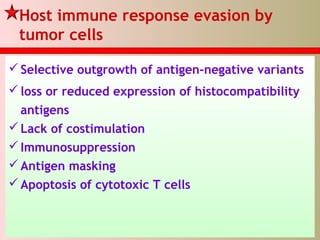
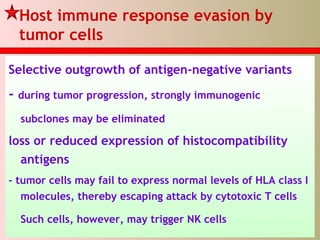
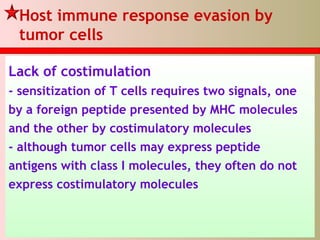
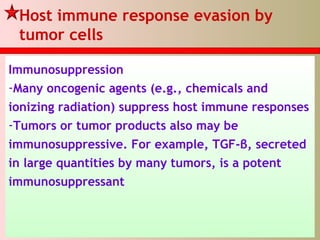
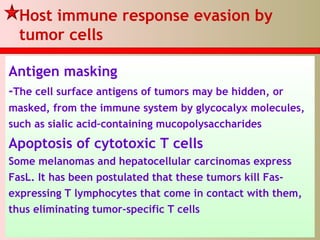
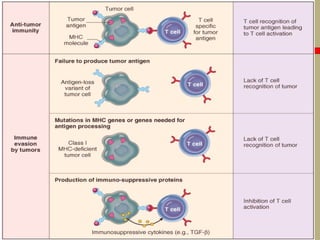
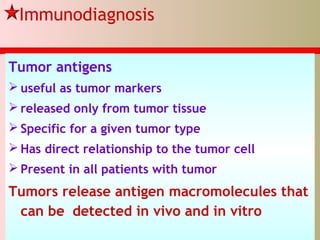
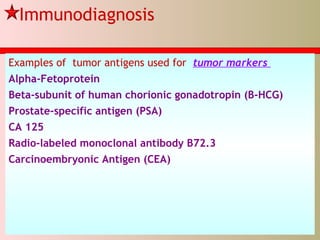
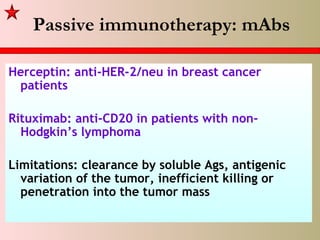
This lecture discusses how the immune system responds to tumors and how tumors evade the immune system. It covers various types of tumor antigens recognized by the immune system, including products of mutated genes, overexpressed proteins, and oncofetal antigens. The immune system mounts cellular and humoral responses against tumors through cytotoxic T cells, NK cells, macrophages, and antibodies. However, tumors have developed mechanisms to evade the immune system, such as antigen loss, lack of costimulation, immunosuppression, and inducing T cell apoptosis. Understanding the immune response and evasion is crucial for developing immunotherapies against cancer.