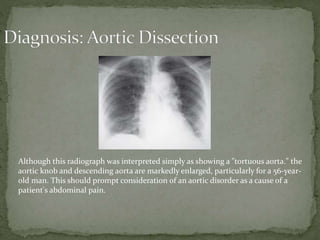
A 56-year-old man presents with 4 hours of epigastric abdominal pain described as sharp and stabbing. He has a history of hypertension and coronary artery disease. On examination, he is tachycardic with cool extremities. Imaging shows an enlarged aorta, particularly for his age, which should prompt consideration of an aortic disorder as the cause of his pain. He requires aggressive blood pressure control and emergent surgical consultation given concern for aortic dissection.