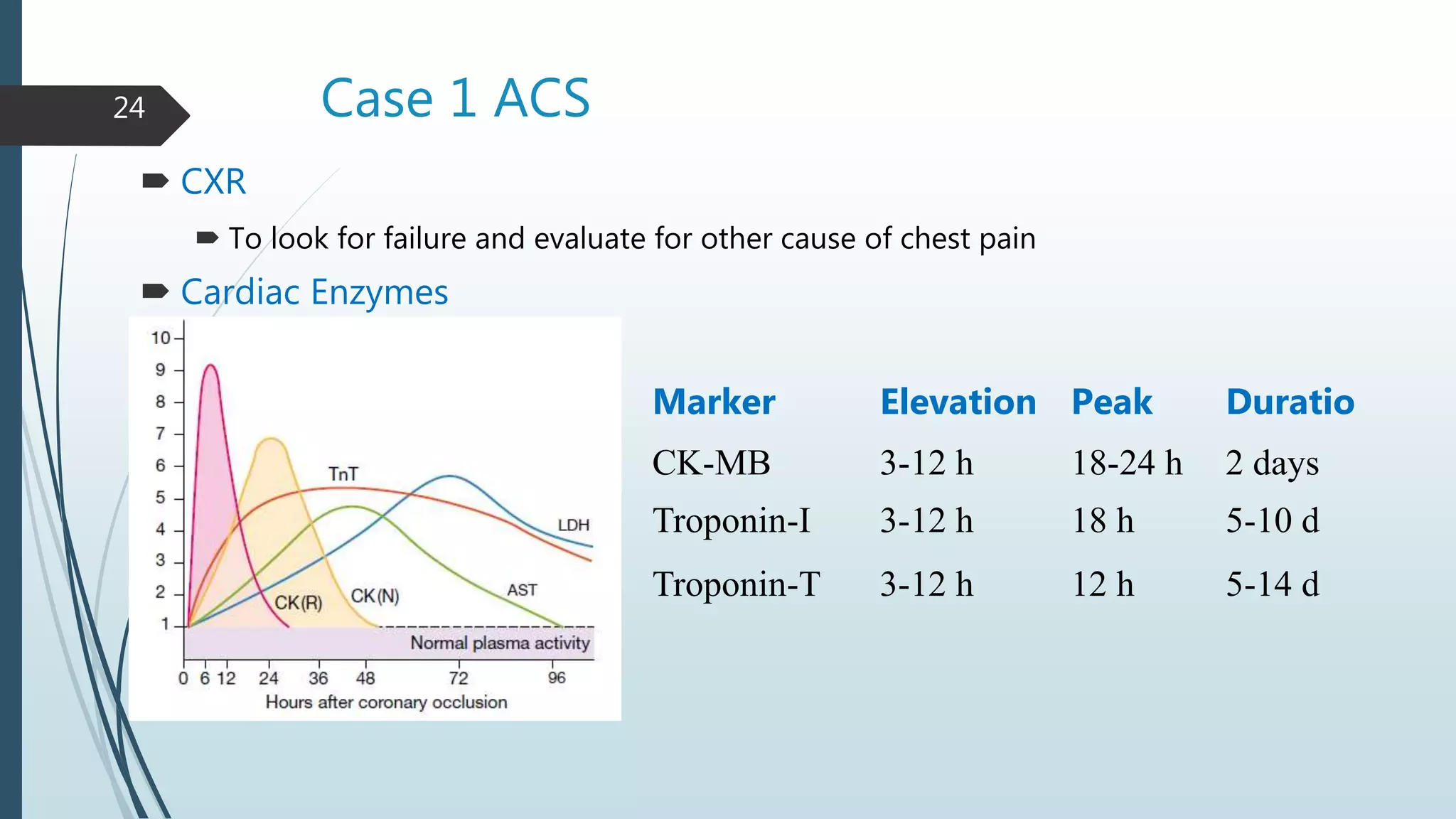
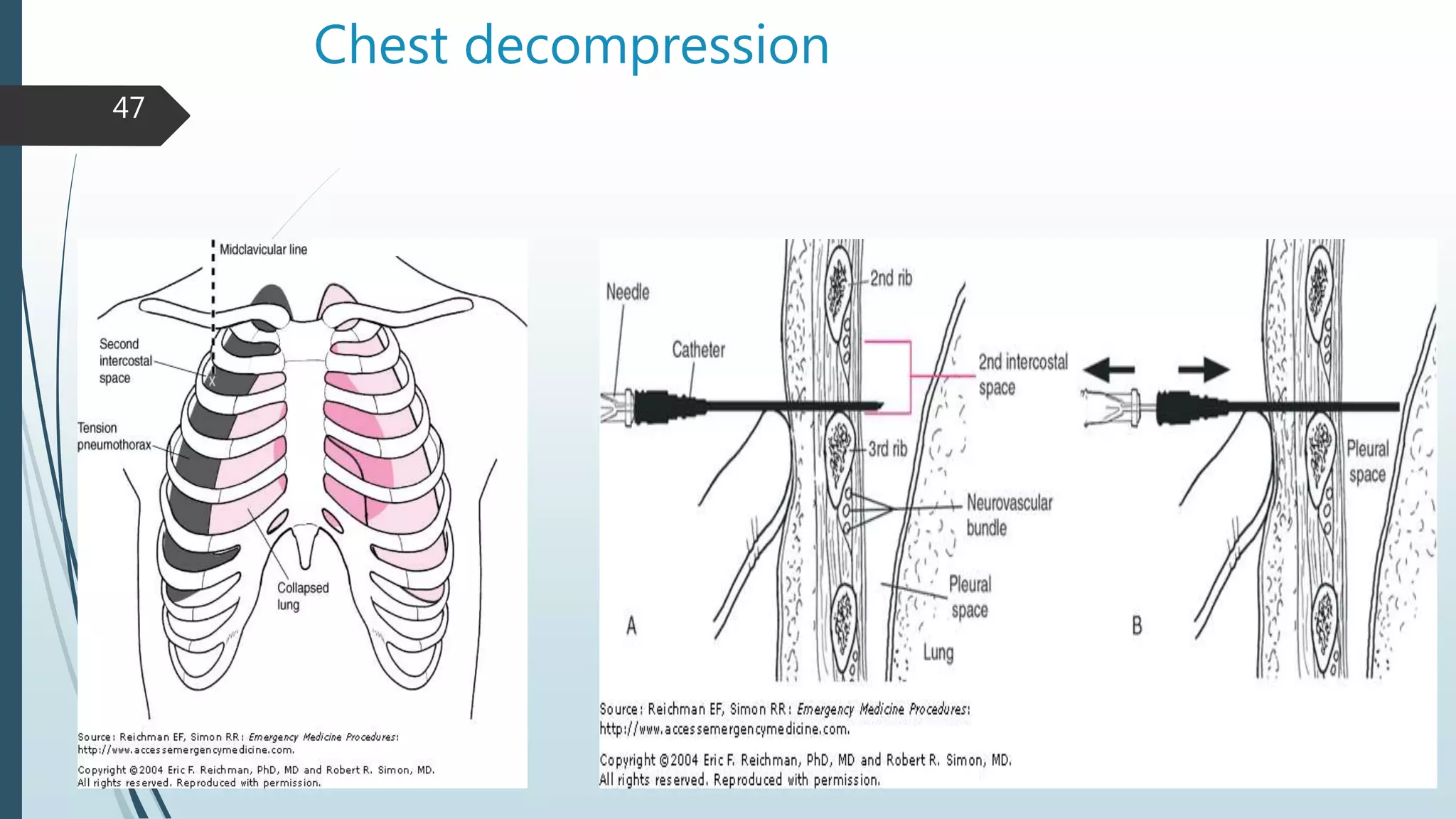
The document discusses chest pain, its various etiologies, types, and management strategies, emphasizing the importance of identifying life-threatening causes like acute coronary syndrome, pulmonary embolism, and aortic dissection. It provides detailed guidelines on patient history, physical examination, diagnostic tests, and treatment protocols. The document also includes case presentations to illustrate the clinical approach to chest pain in emergency settings.