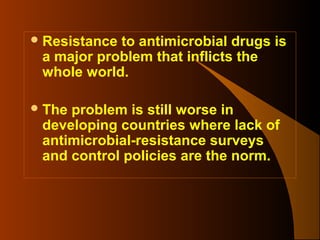
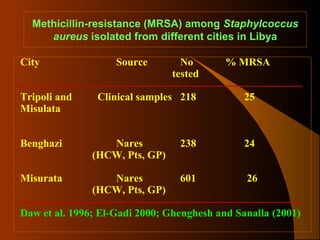
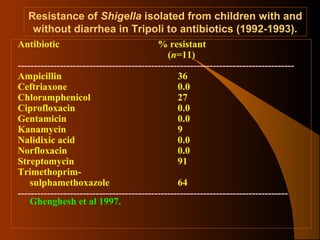
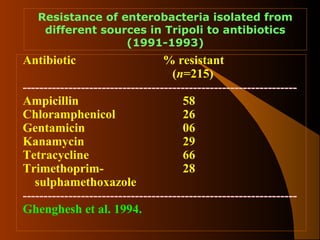
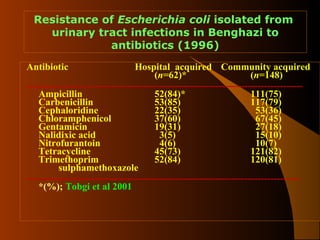
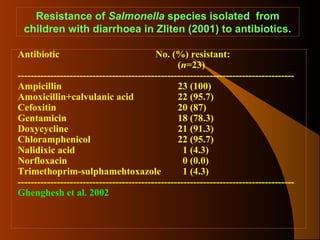
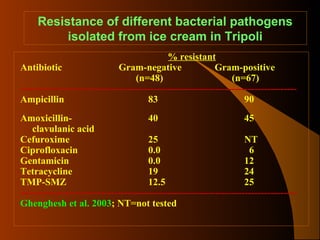
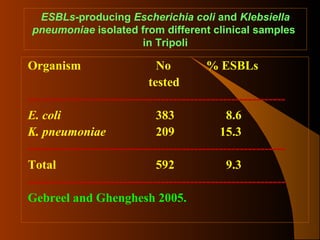
This document discusses antimicrobial resistance in Libya. It finds resistance is a serious problem that is increasing, including emerging resistance to newer drugs. Many bacteria isolated from clinical and other sources in Libya show high resistance percentages to various antibiotics. Resistance appears related to easy over-the-counter antibiotic access without prescription, improper hospital usage, and uncontrolled animal antibiotic use. Urgent action is needed to regulate antibiotic sales and usage, educate on proper clinical use, control hospital infections, and regulate non-human antibiotic use to address this growing resistance issue in Libya.