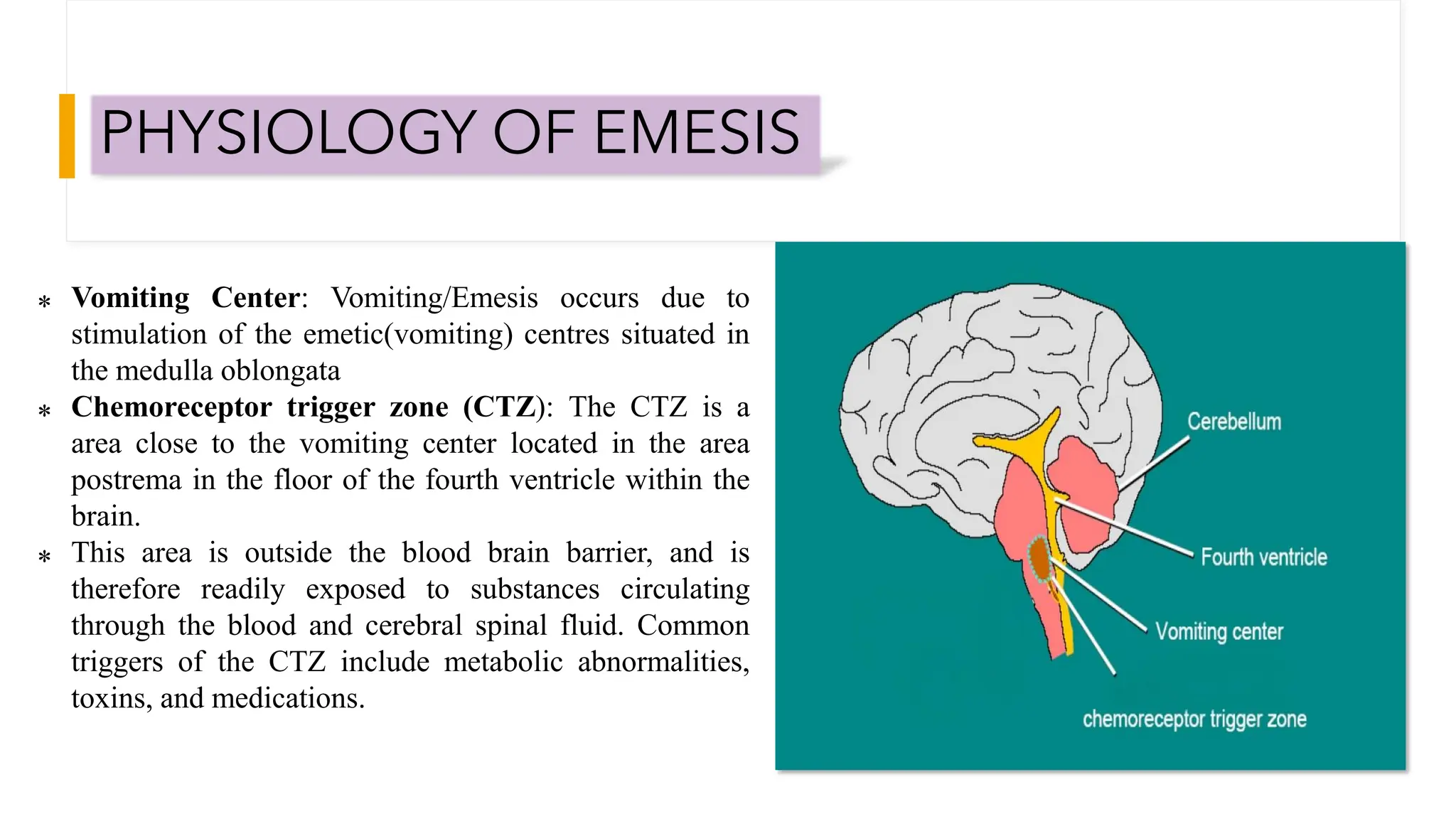
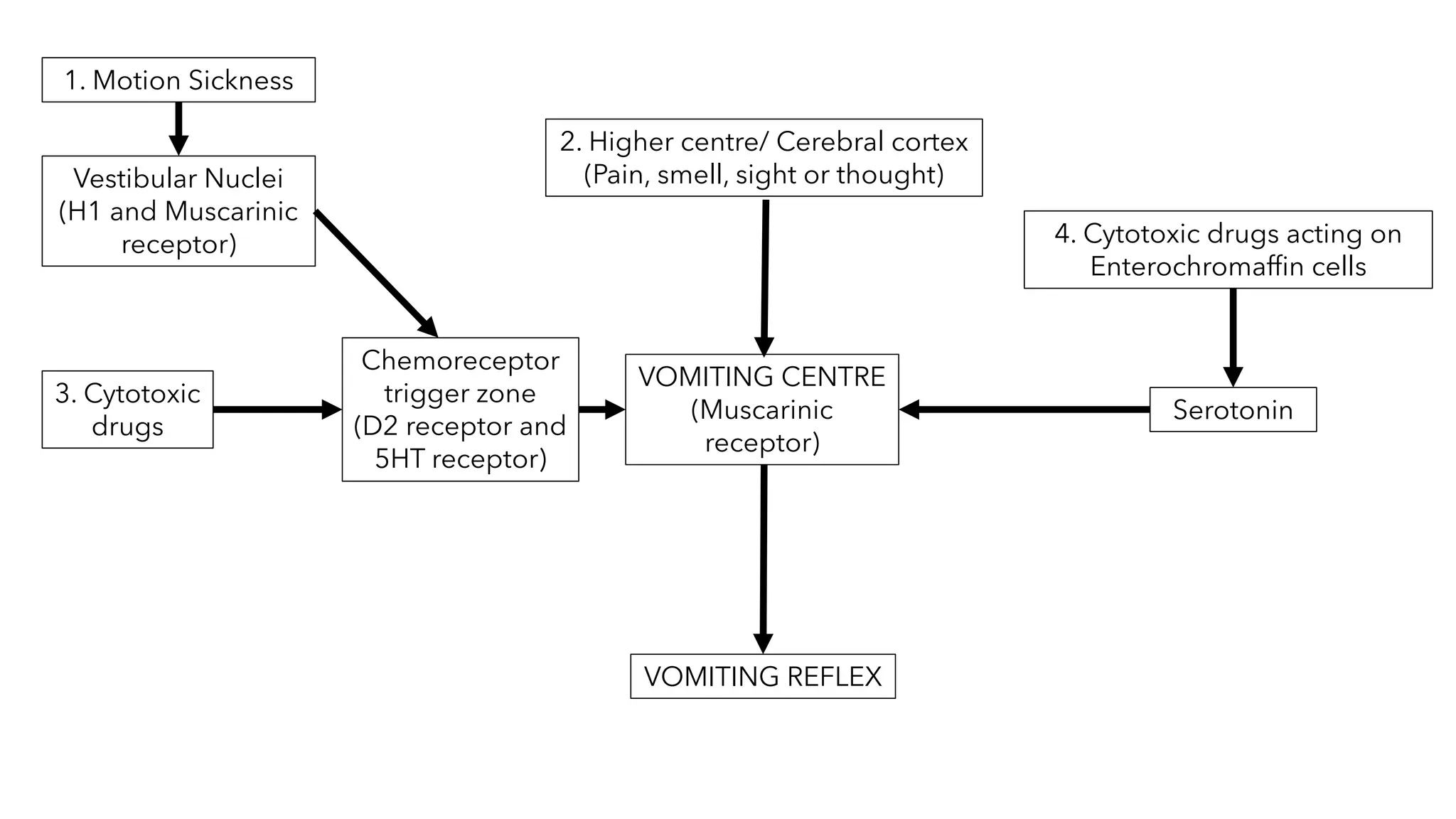
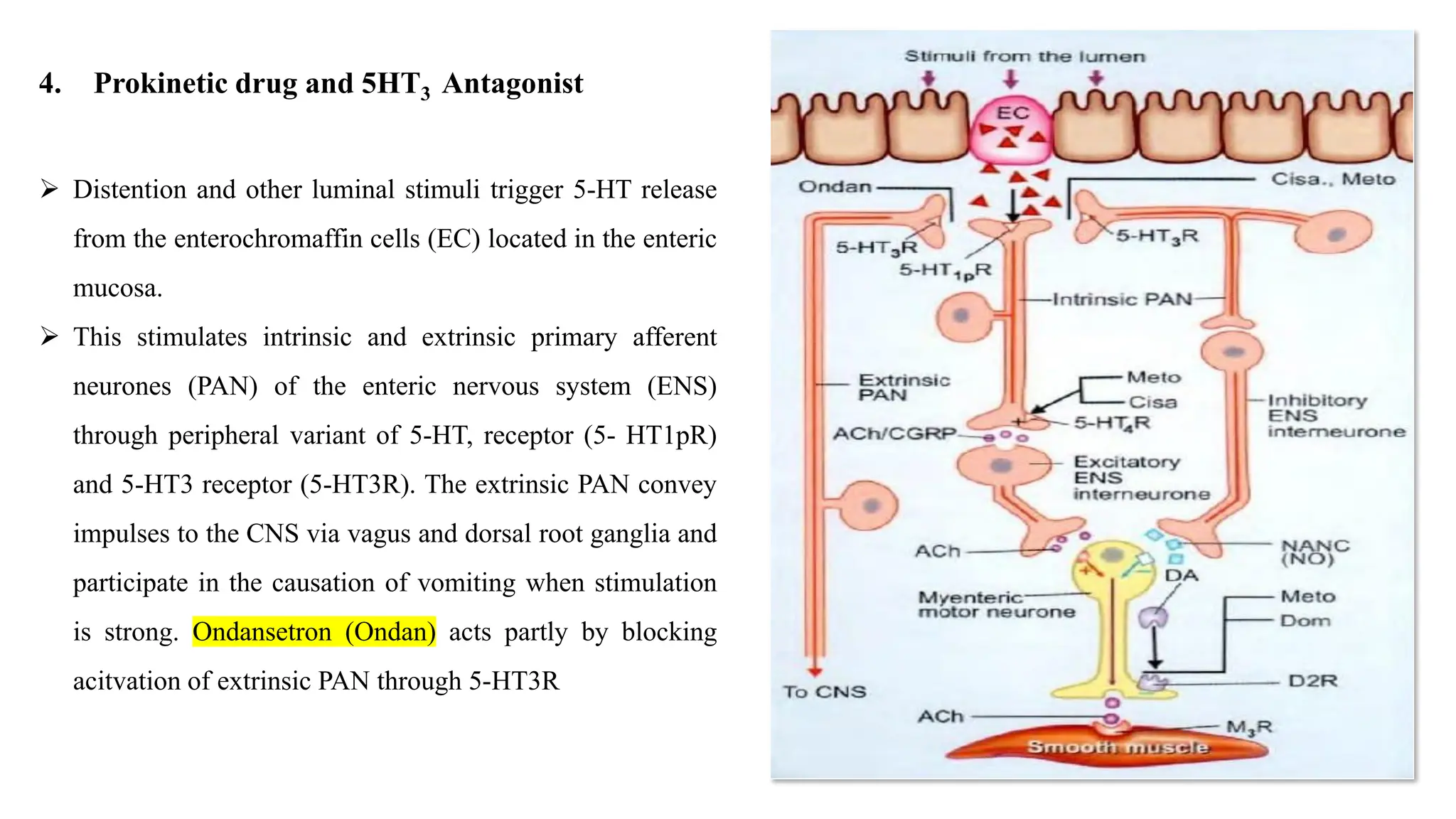
This document presents information about antiemetics, including their classification and mechanisms of action. It begins with an introduction to emesis and the types of vomiting. It then discusses the physiology of vomiting, including the vomiting center and chemoreceptor trigger zone in the brain. The document categorizes and describes various classes of antiemetics like anti-cholinergics, H1 antihistamines, neuroleptics, prokinetic drugs, 5-HT3 antagonists, and adjuvant antiemetics. It provides examples of drugs in each class and explains their mechanisms of action, primarily involving the blocking of receptors in the brain and gastrointestinal tract to prevent nausea and vomiting.