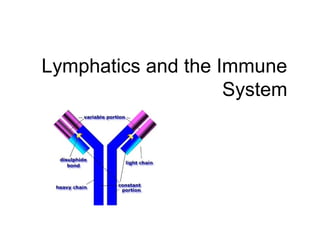
The document describes the lymphatic system and immune system. It explains that the lymphatic system is made up of lymph vessels and lymph nodes that collect and filter excess fluid in the body. The immune system protects the body through innate defenses like physical barriers and inflammatory responses, as well as through adaptive defenses involving lymphocytes that provide long-lasting immunity.