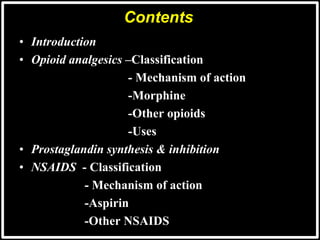
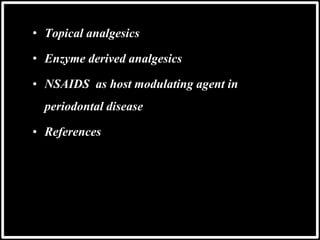
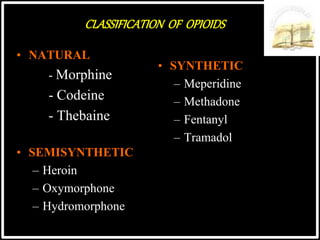
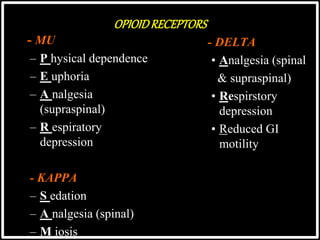
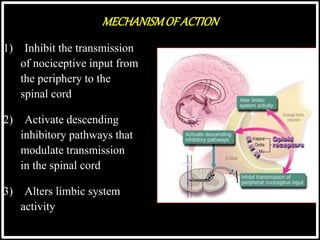
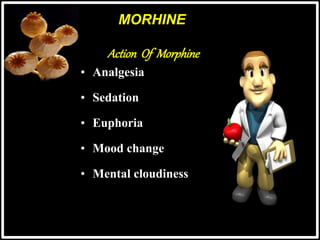
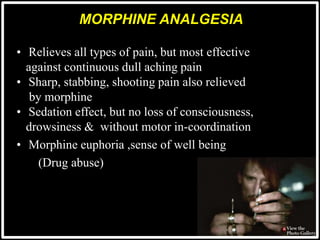
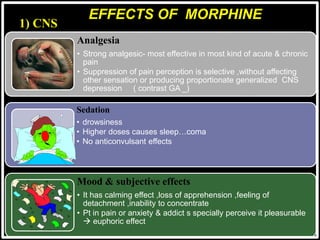
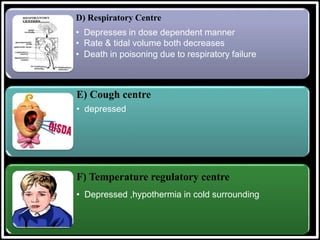
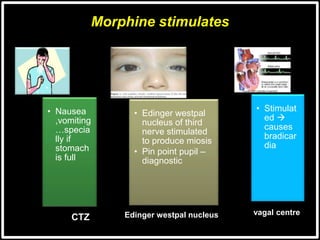
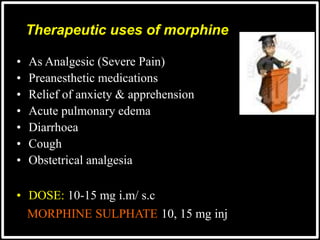
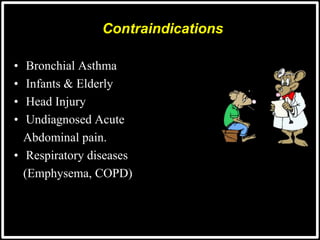
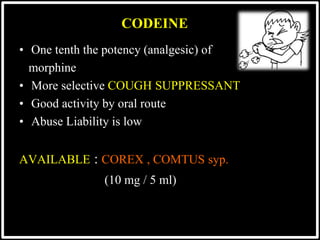
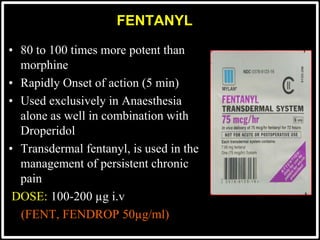
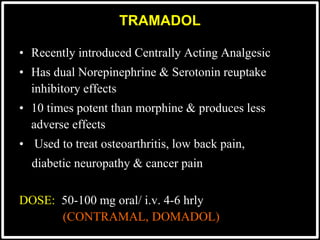
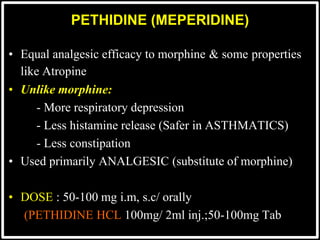
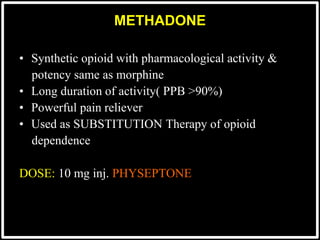
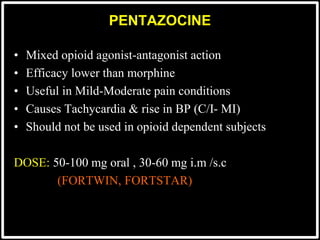
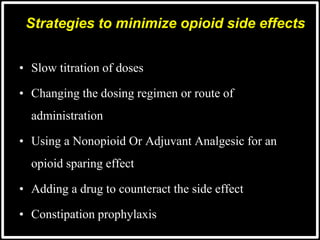
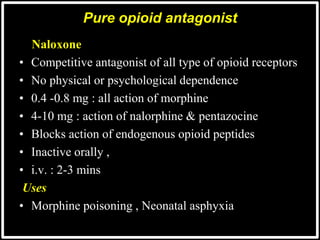
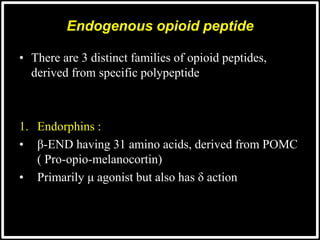
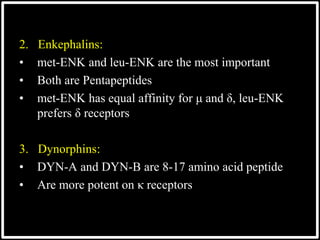
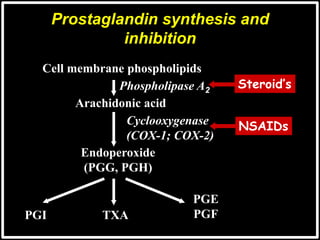
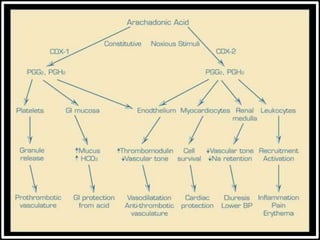
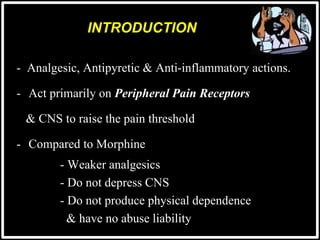
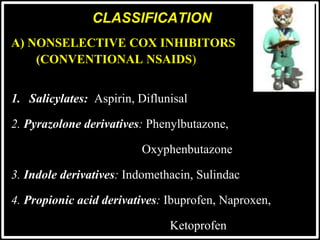
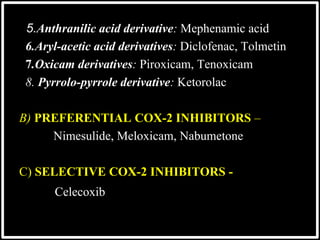
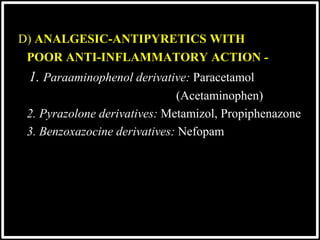
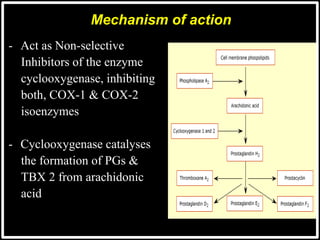
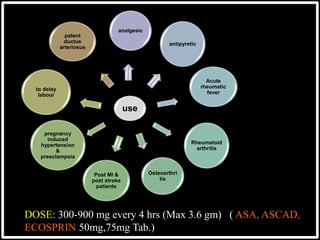
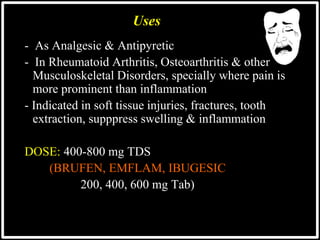
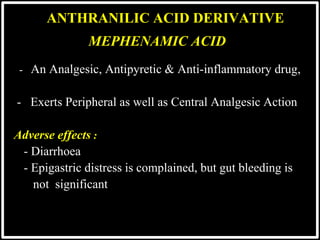
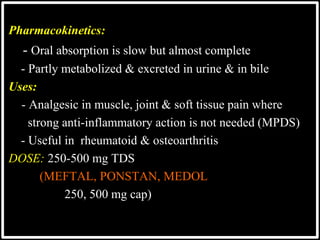
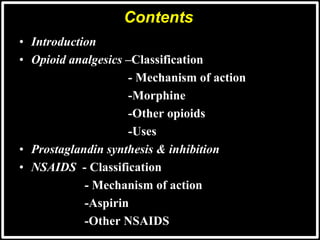
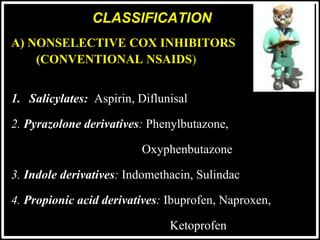
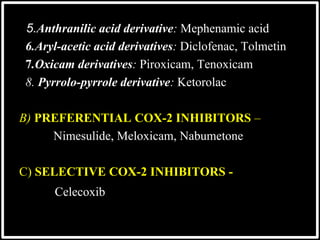
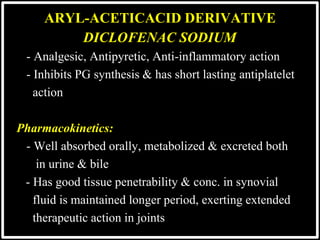
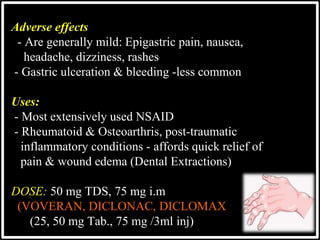
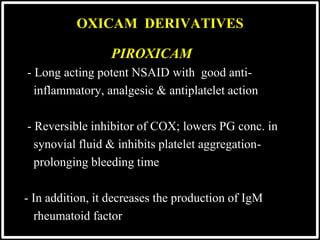
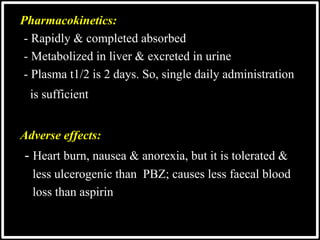
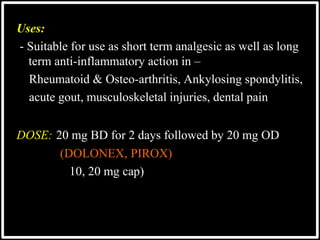
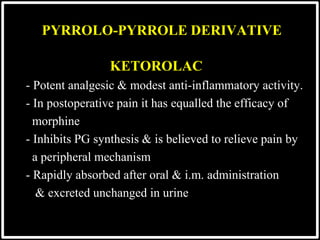
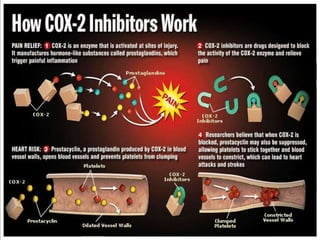
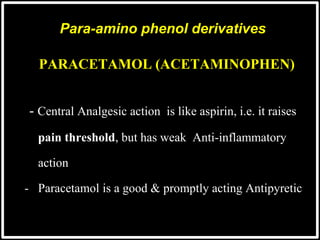
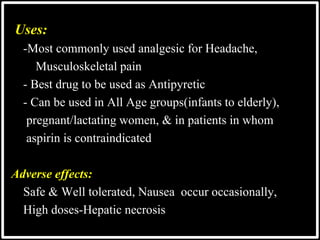
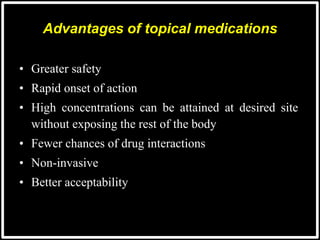
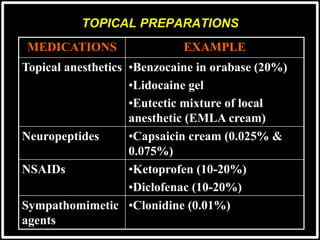
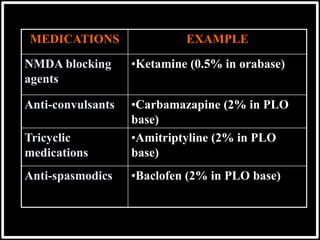
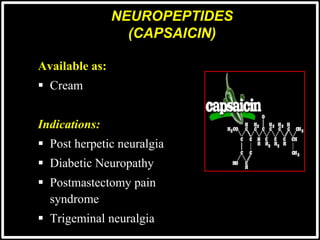
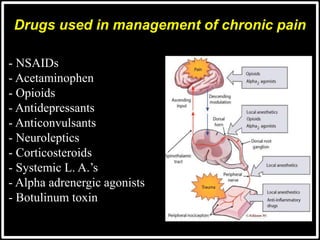
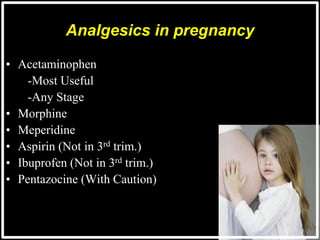
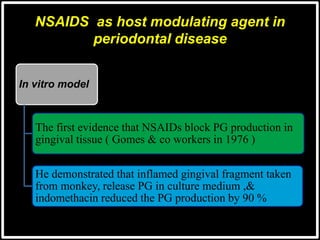
This document provides an overview of analgesics, including opioids and NSAIDs. It discusses the classification, mechanisms of action, uses, and side effects of various opioid analgesics like morphine, codeine, fentanyl, tramadol, pethidine, and methadone. It also summarizes the classification of NSAIDs, how they work by inhibiting prostaglandin synthesis, and examples like aspirin. The document defines pain and the management of pain using topical, systemic and other analgesic medications.