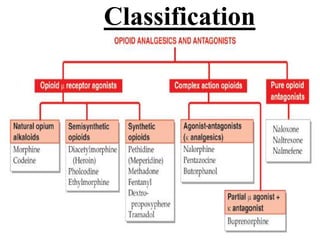
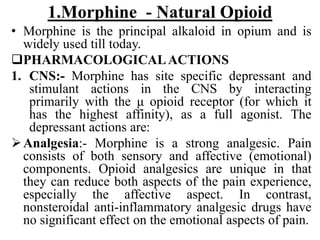
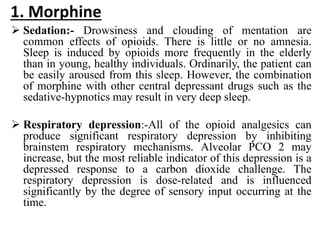
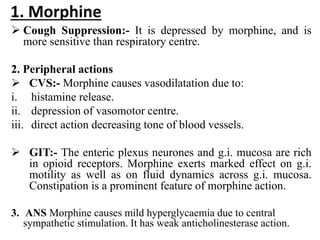
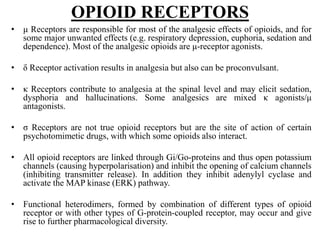
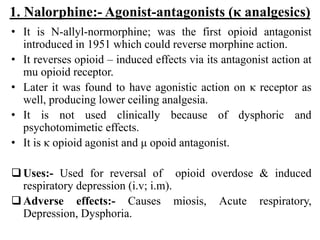
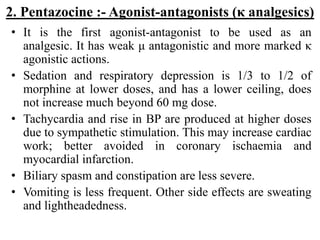
This document provides an overview of narcotic analgesics, focusing on their definitions, classifications, and pharmacological effects. It discusses various opioids, including morphine, codeine, fentanyl, tramadol, and their therapeutic uses, adverse effects, and mechanisms of action. The document highlights the differences between opioid and non-opioid analgesics, as well as the implications of drug interactions and the role of opioid receptors.