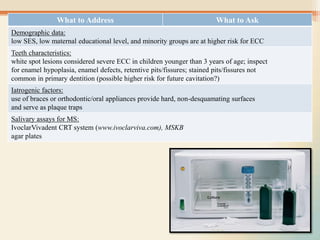
This document discusses preventive strategies in pediatric dentistry. It outlines how the old infectious disease model was deficient and has been replaced by anticipatory guidance. Anticipatory guidance provides age-specific counseling to parents on oral development, diet, fluoride, habits, hygiene, and injury prevention. It aims to address protective factors to prevent oral health problems. Starting prevention early in infancy allows for developing an individualized plan. To be effective, anticipatory guidance should be coupled with oral health risk assessment and caries risk tools to properly evaluate risk factors and customize prevention.