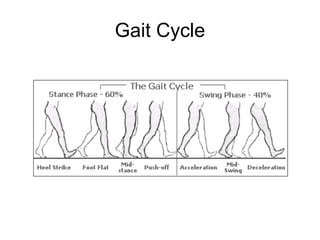
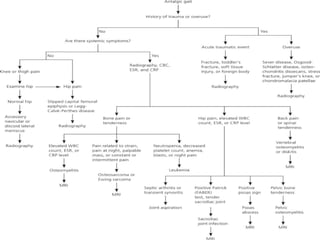
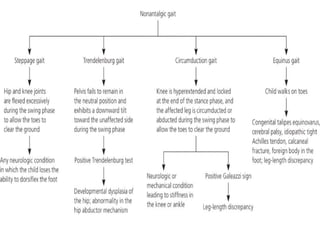
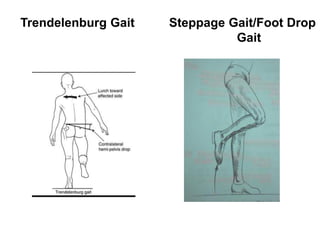
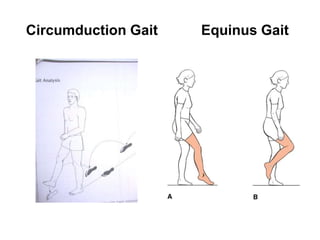
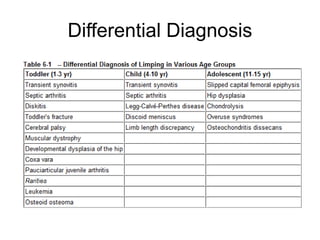
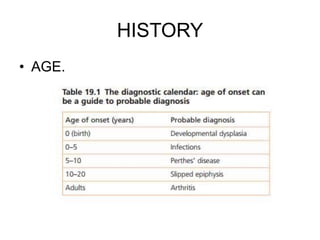
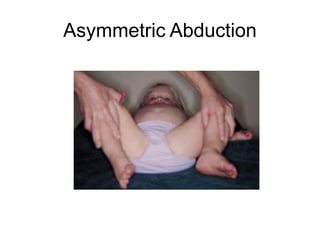
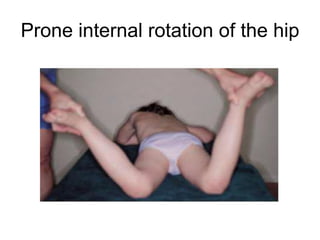
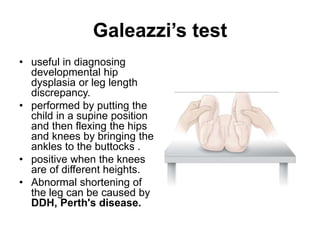
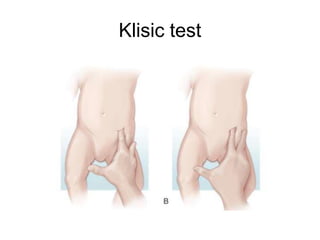
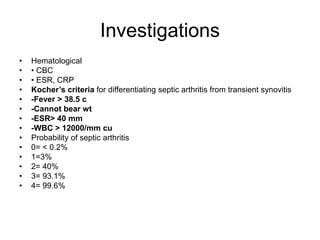
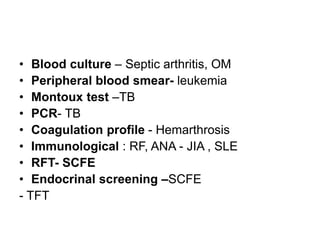
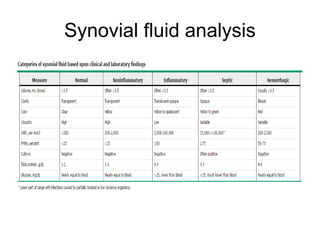
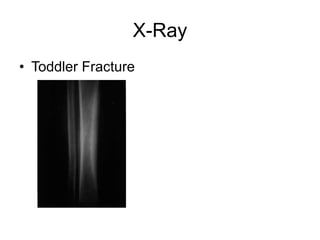
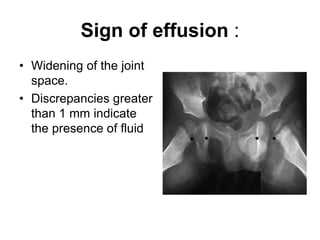
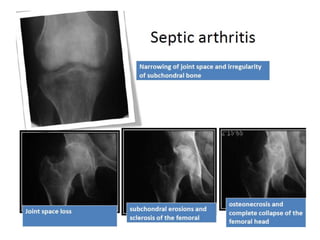
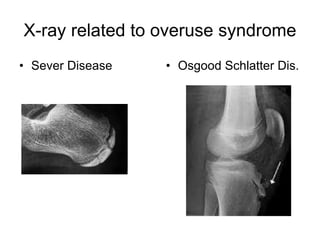
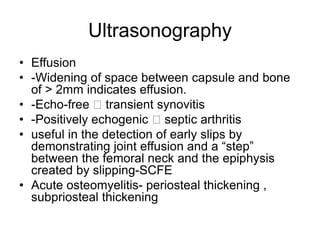
This document provides guidance on evaluating a limping child. It discusses that limp can be caused by pain, weakness or deformity and management depends on the underlying cause. A thorough history, physical exam, and investigations may be needed. The physical exam involves assessing gait, leg length, range of motion, and neurological function. Potential investigations include blood tests, imaging like x-rays, ultrasound and MRI to identify causes such as fractures, infections, tumors or developmental disorders. The goal is to determine the cause and provide appropriate treatment ranging from reassurance to surgery.