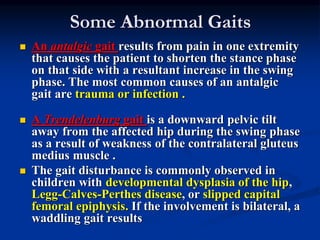
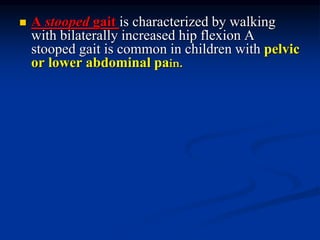
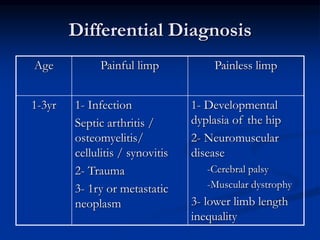
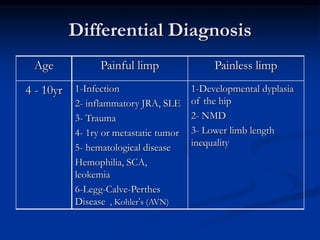
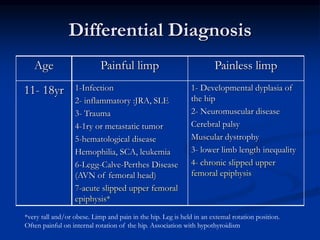
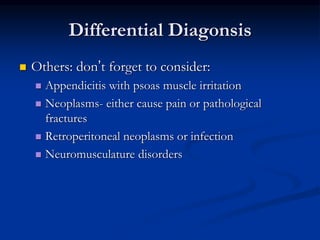
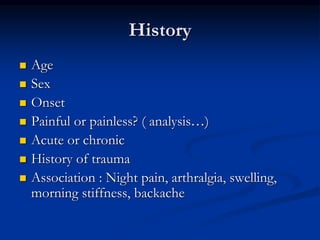
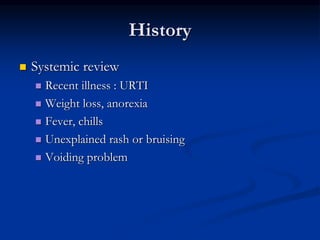
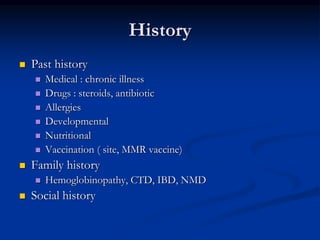
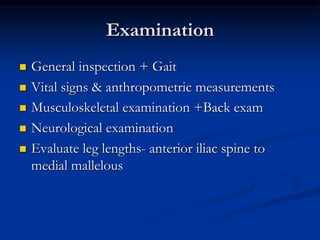
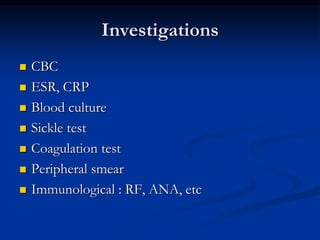
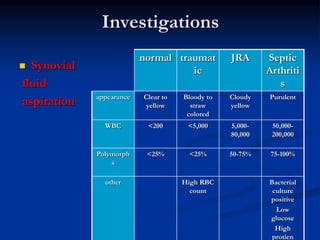
This document discusses the approach to evaluating a limping child. It begins by outlining the main causes of a limp as being pain, weakness, or structural abnormalities. Different abnormal gaits are then described that may provide clues to the underlying etiology, such as an antalgic gait indicating pain in one limb. A differential diagnosis is presented divided by painless versus painful limps and by age. The approach is then outlined as obtaining a thorough history, performing a full examination, ordering appropriate investigations, and determining the proper management.