The document discusses various memory disorders, focusing on age-associated memory impairment (AAMI) and dementia, particularly Alzheimer's disease. It outlines the characteristics, symptoms, and diagnostic criteria for these conditions, along with differences between organic and psychogenic amnesias. Additionally, it highlights the implications of HIV-related cognitive disorders and the importance of management strategies, including the use of highly active antiretroviral therapy (HAART).
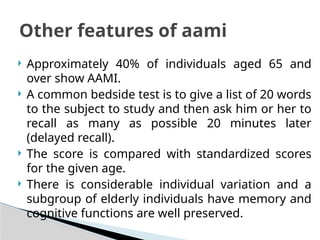
![ In a study of patients with HIV in a Ugandan clinic,
the prevalence of ADC was 31%.
If extrapolated to sub-Saharan Africa (26 million
people with HIV out of 40.3 million people
infected worldwide), ADC would be the most
important cause of dementia in persons younger
than 40 years.
The incidence of AIDS dementia is low when
access to health care is good; risk factors include
non-use of HAART and low CD4+
counts.[28]
Incidence in sub saharan
africa](https://image.slidesharecdn.com/lect6memorydisoders-240924160124-31db6826/85/LECT-6-MEMORY-DISODERS-pptx-41-320.jpg)