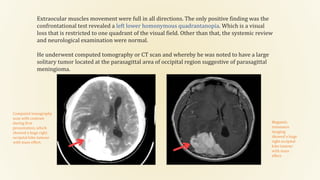
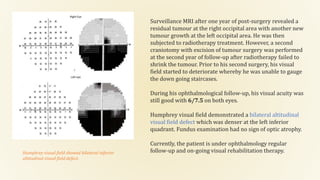
The document describes a rare case of bilateral inferior altitudinal visual field defect (biavfd) caused by a recurrent occipital meningioma in a 52-year-old male patient. Despite normal visual acuity and unremarkable optic nerve examinations, the patient exhibited significant visual field defects associated with his tumor, which was later confirmed through imaging. The case highlights the need for timely diagnosis and management, including rehabilitation strategies to improve patients' quality of life following visual impairments.