This document provides an overview of alcoholic liver disease (ALD). It discusses the introduction, etiology, pathogenesis, clinical features, diagnosis, prognosis, and treatment of ALD. The key points are:
1) ALD is responsible for 50% of cirrhosis mortality and is the 3rd largest risk factor for disease burden worldwide.
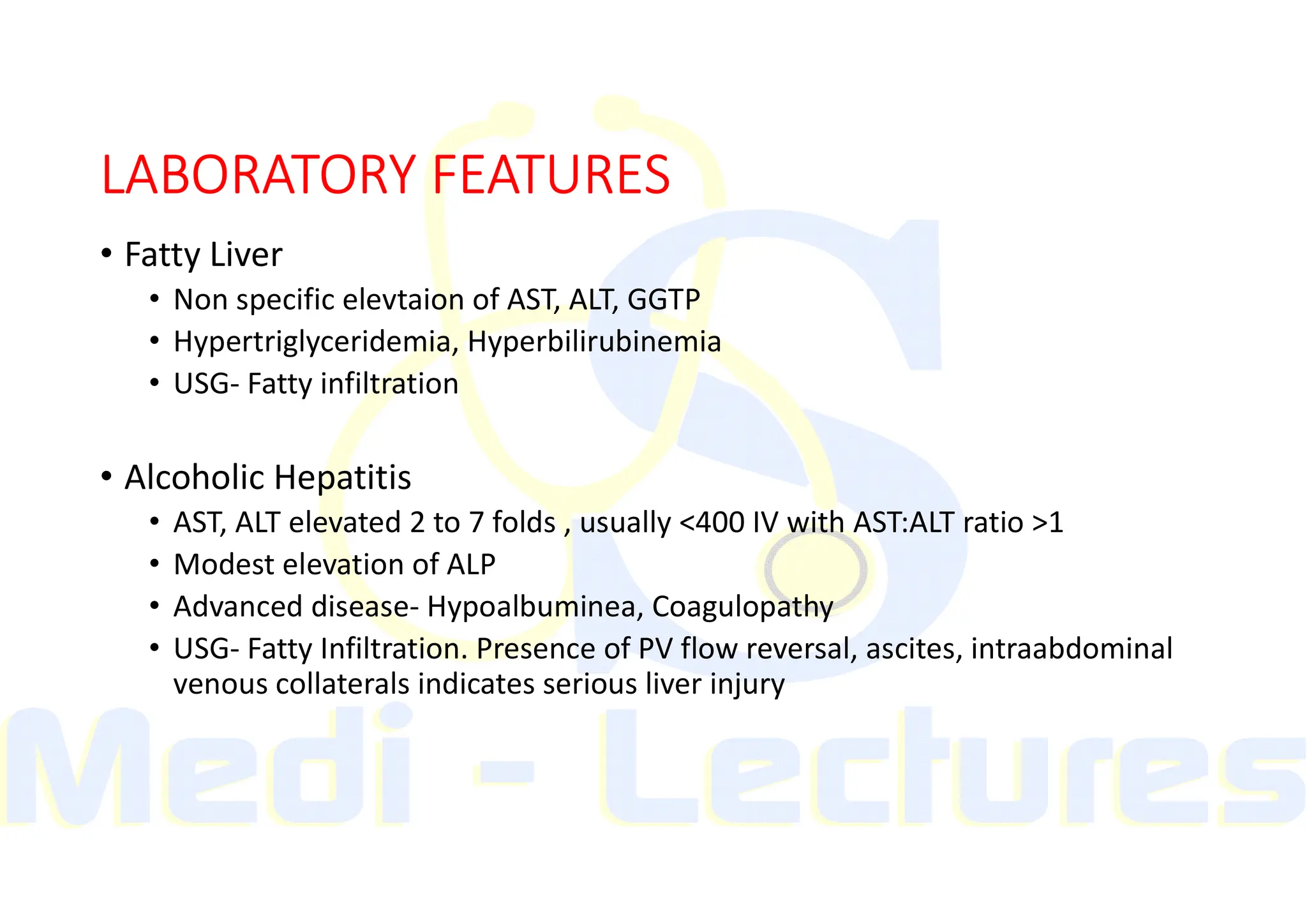
2) The amount and duration of alcohol consumption are the most important risk factors. Chronic heavy drinking leads to fatty liver, alcoholic hepatitis, and cirrhosis over time.
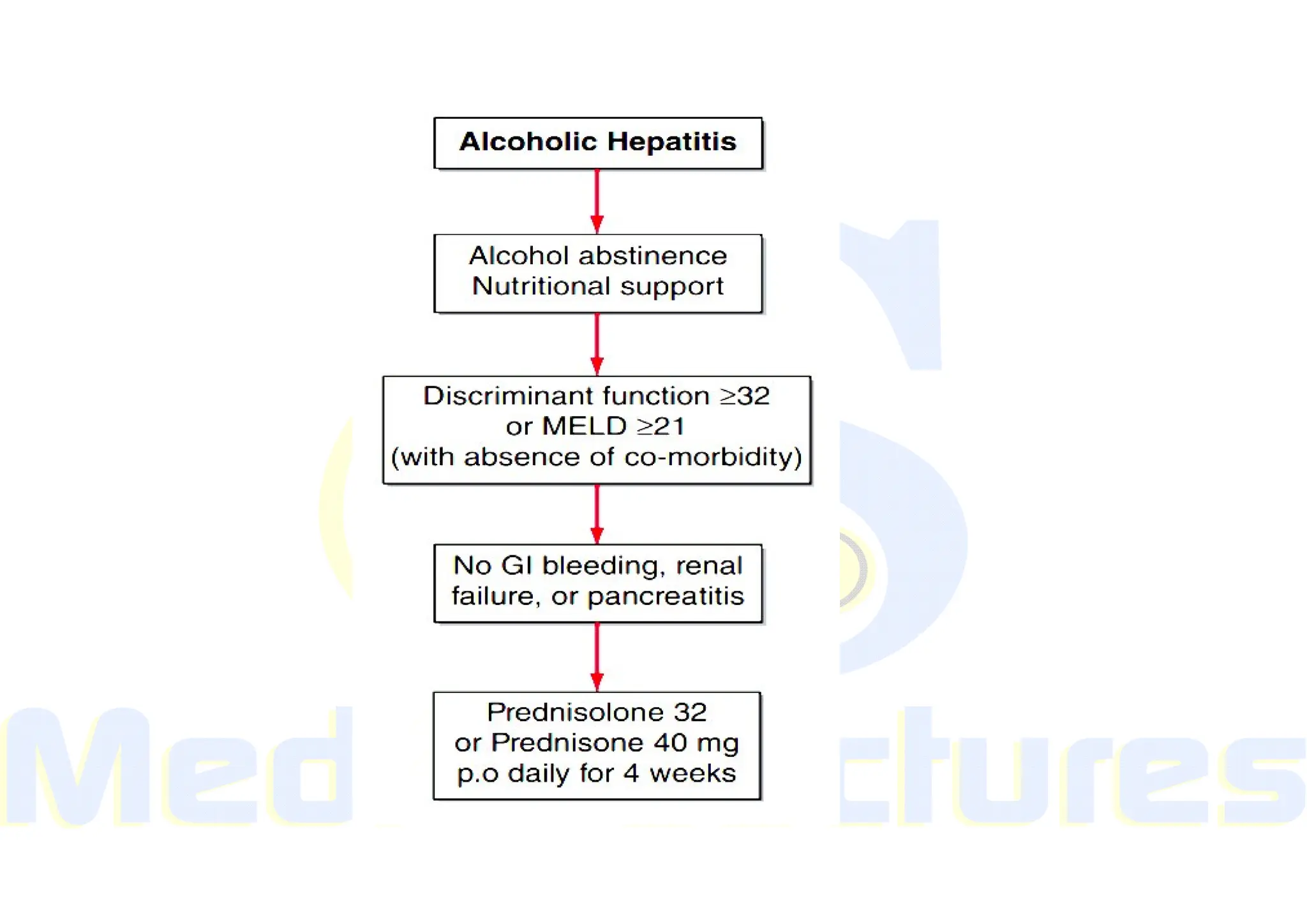
3) Treatment involves complete alcohol abstinence. Glucocorticoids or pentoxifylline may be used for severe alcoholic hepatitis. Liver transplantation is an option for end-