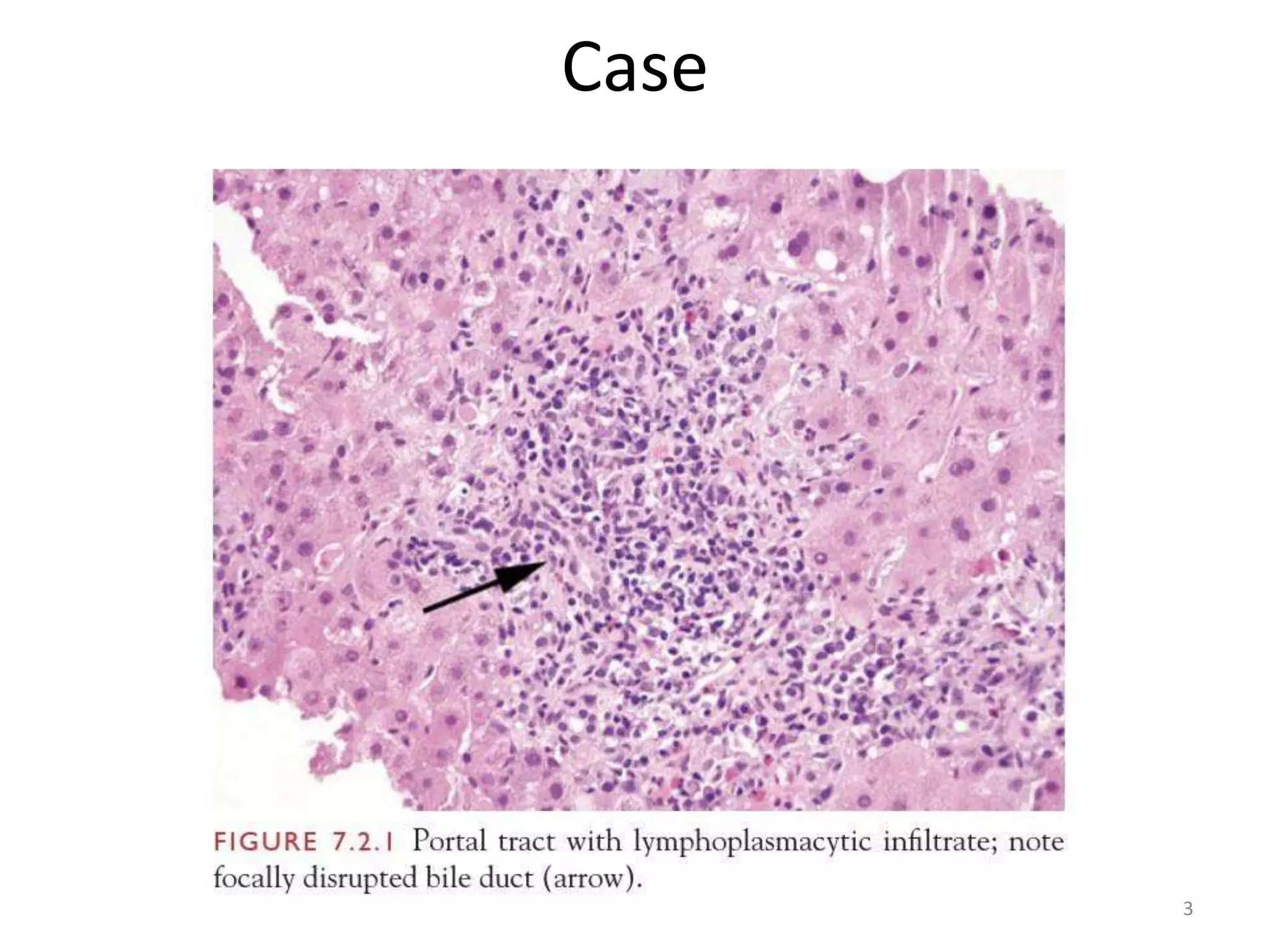
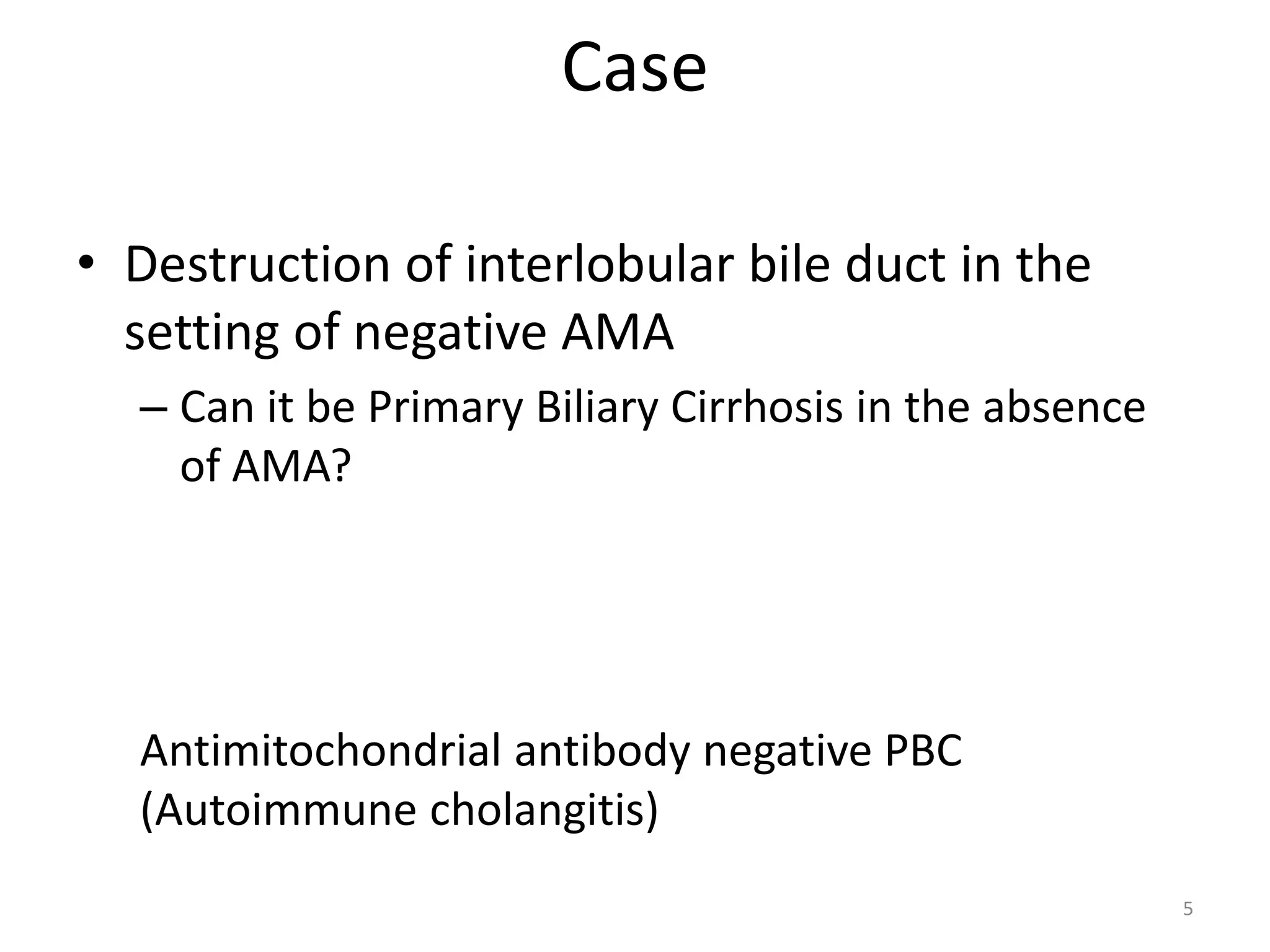
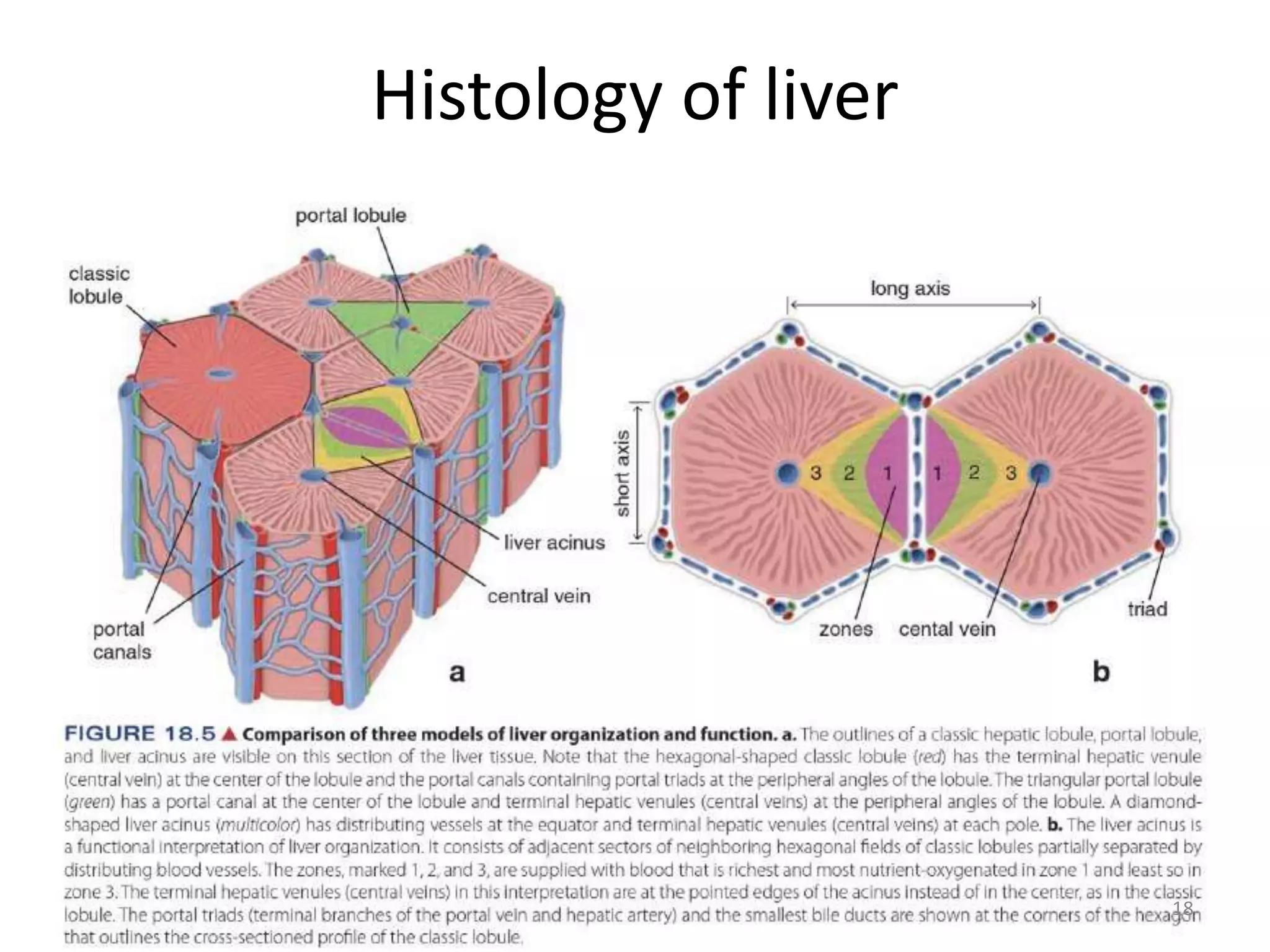
This document provides a summary of a histology presentation on liver biopsy and various liver diseases. It discusses 5 cases presented as examples. It then covers topics of liver biopsy techniques and specimen handling. An overview of examining liver biopsy specimens under the microscope is provided. Key aspects of normal liver histology and histological features of fatty liver disease, alcohol-induced liver disease, and primary biliary cirrhosis are summarized. Diagrams and photomicrographs supplement the textual descriptions.