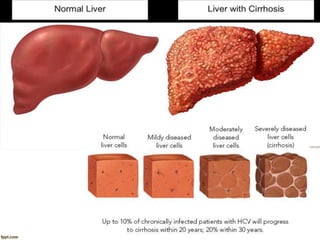
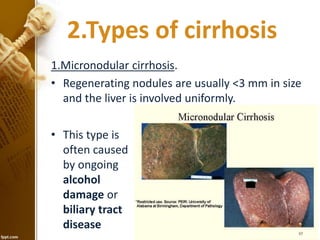
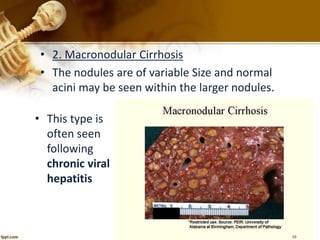
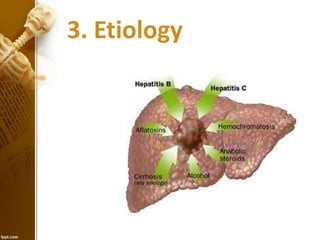
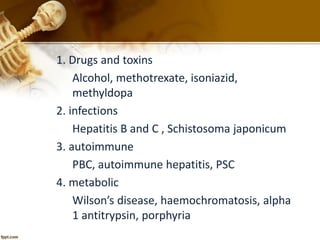
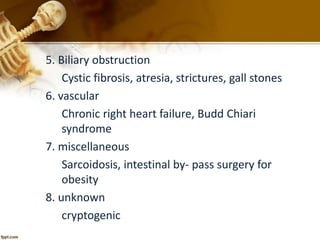
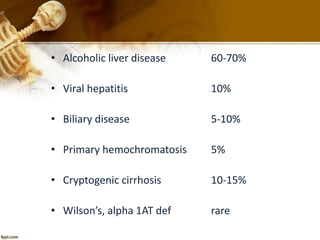
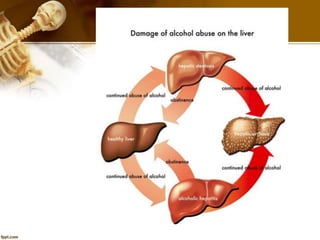
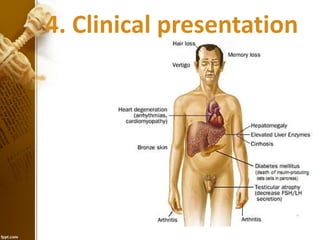
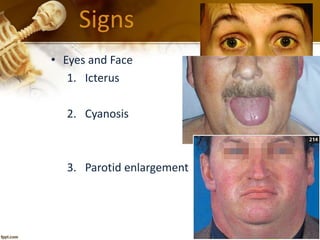
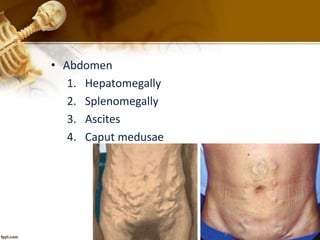
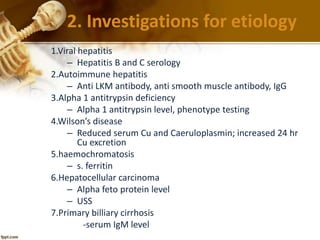
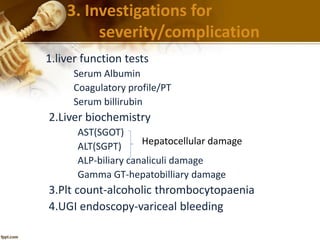
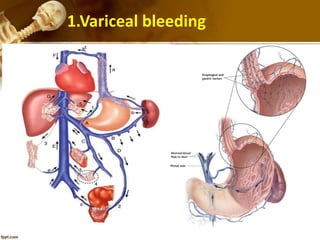
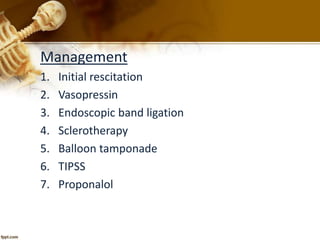
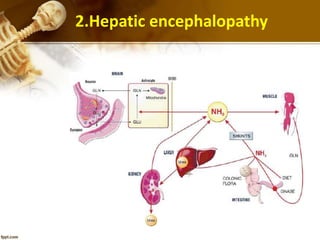
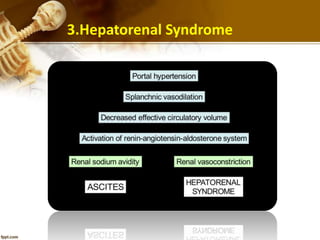
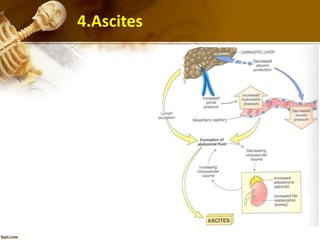
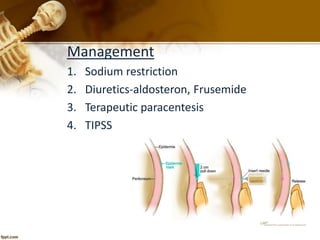
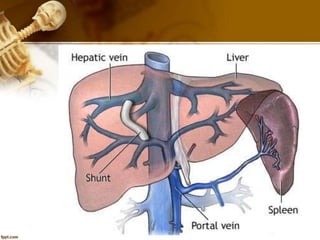
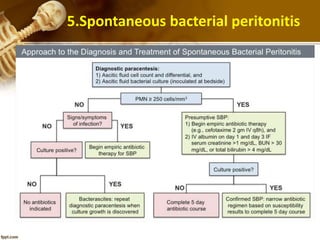
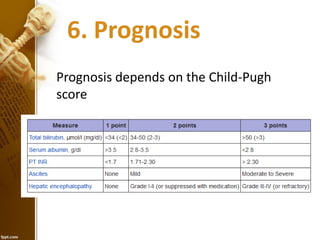
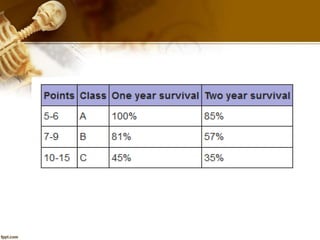
Cirrhosis is a chronic liver disease characterized by fibrosis and loss of liver function, with types including micronodular and macronodular cirrhosis, often due to factors like alcohol, viral infections, and metabolic disorders. Clinical presentation varies and includes non-specific symptoms like malaise and jaundice, alongside distinct physical signs and complications. Management encompasses supportive care, addressing specific etiologies, and treatment of complications, with prognosis evaluated via the Child-Pugh scoring system.