The document discusses alcohol use disorders and management. Some key points:
- Alcohol use results in 2.5 million deaths annually worldwide, especially among youth.
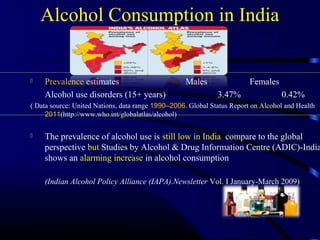
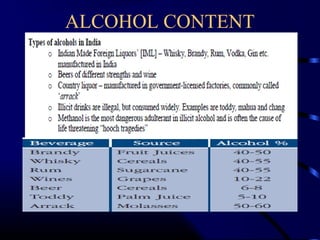
- India's alcohol consumption is increasing, especially in certain states, and the average age of initiation is declining.
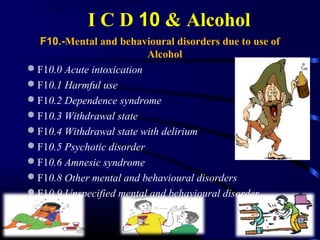
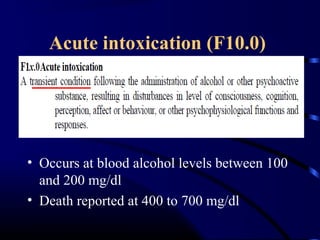
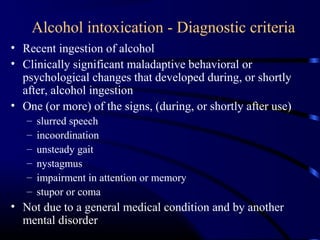
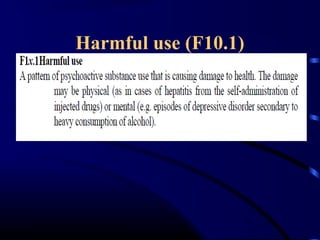
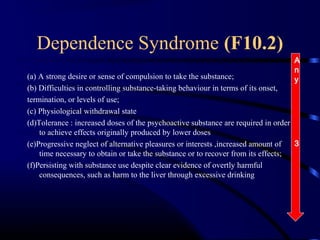
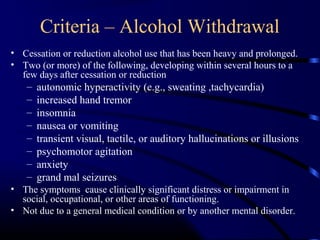
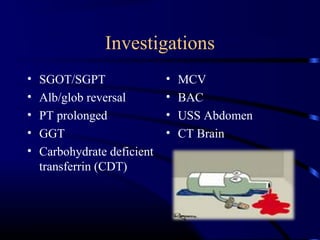
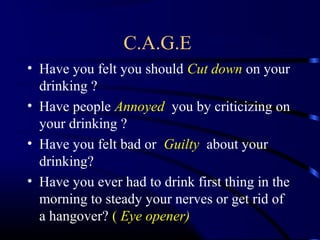
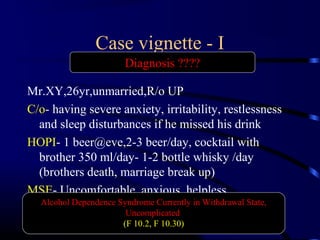
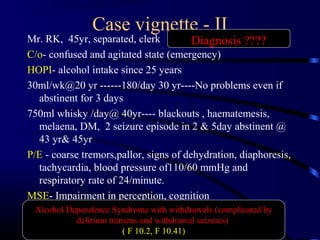
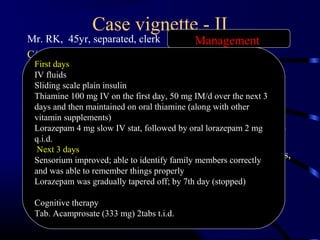
- Alcohol dependence is diagnosed based on criteria including withdrawal symptoms and tolerance.
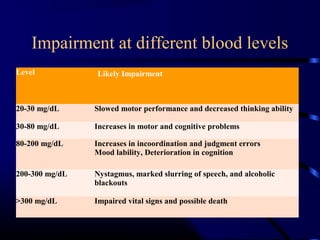
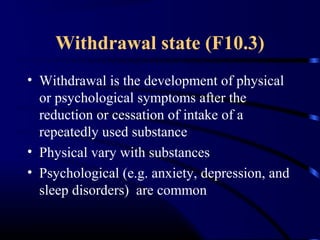
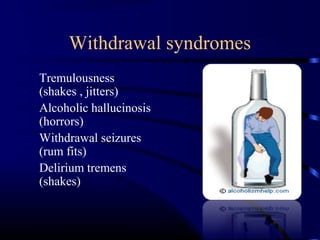
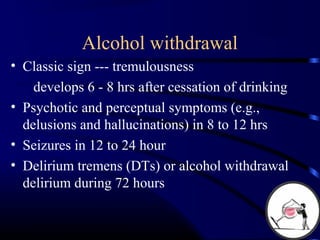
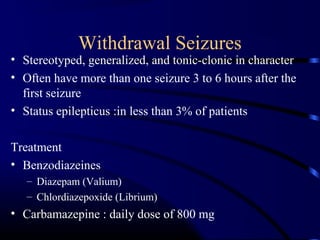
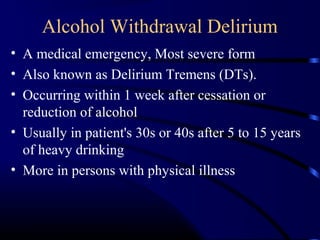
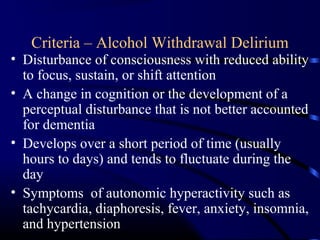
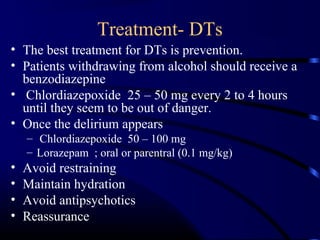
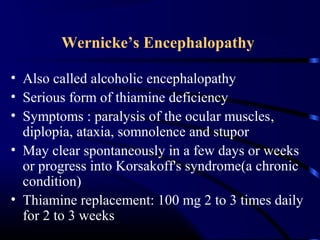
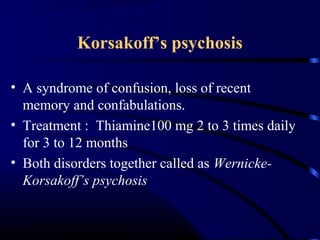
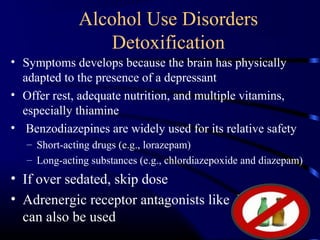
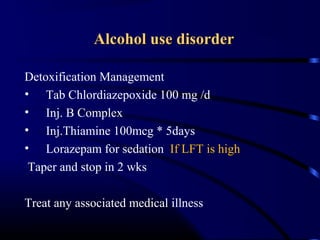
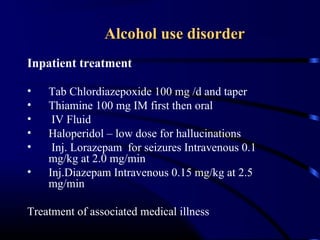
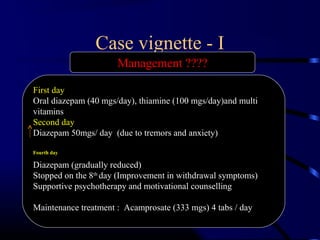
- Withdrawal can cause tremors, seizures, delirium tremens and is managed with benzodiazepines.
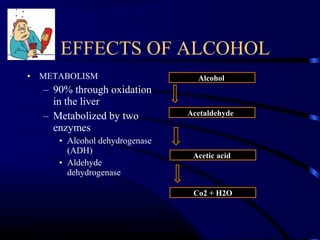
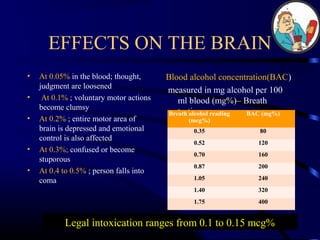
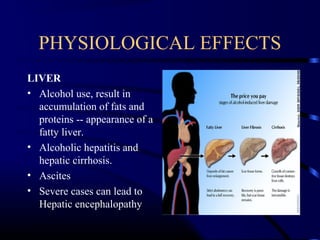
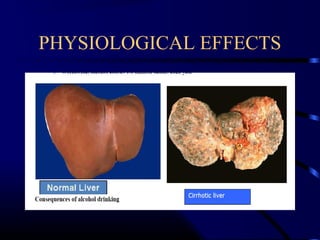
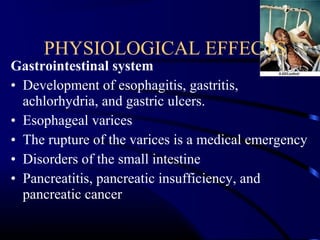
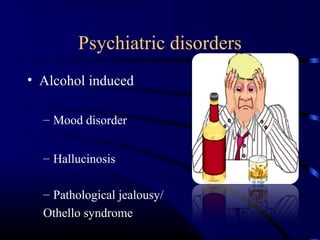
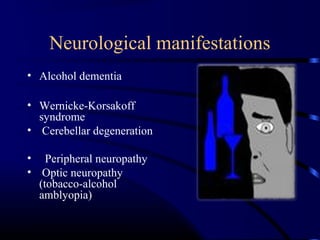
- Long-term effects include liver disease, brain damage and increased risk of certain cancers.