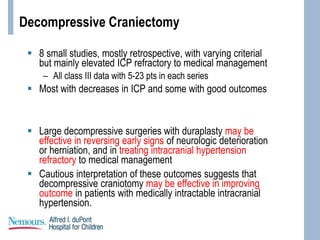
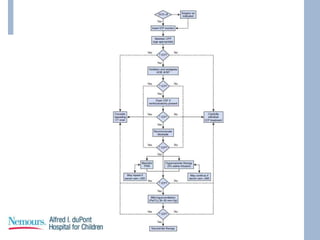
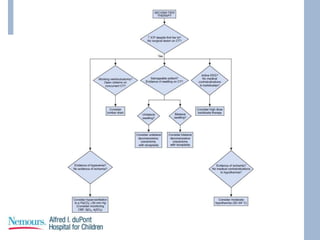
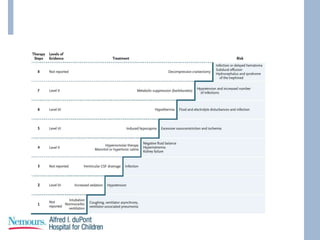
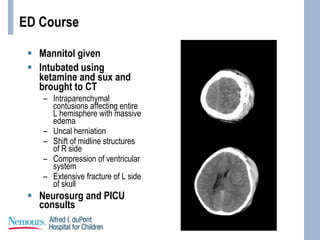
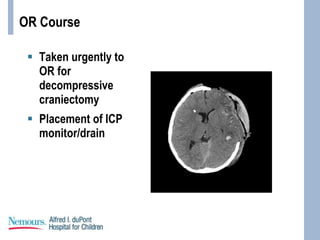
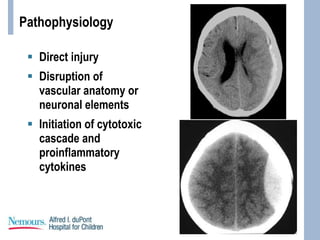
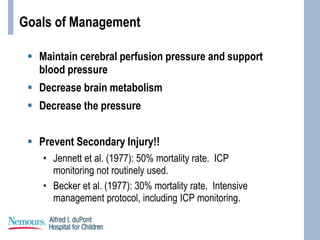
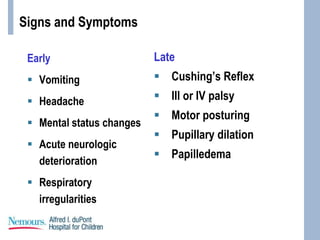
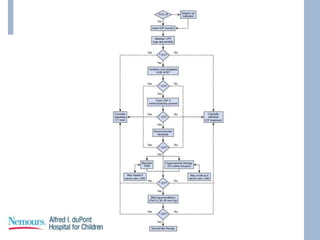
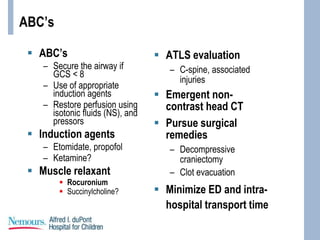
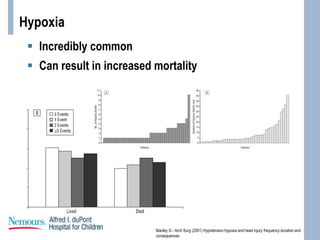
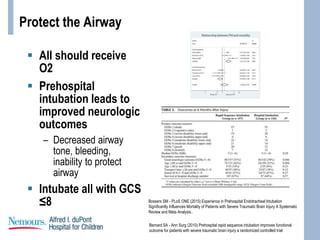
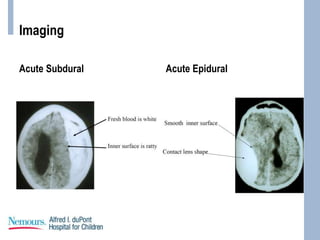
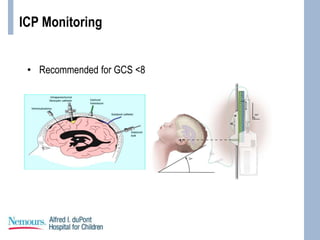
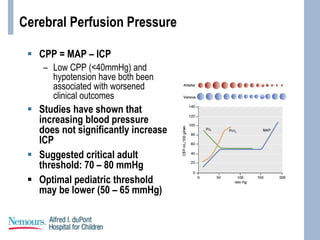
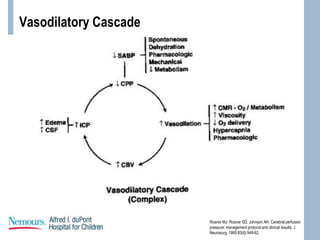
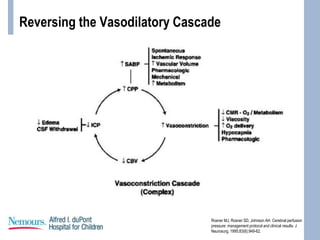
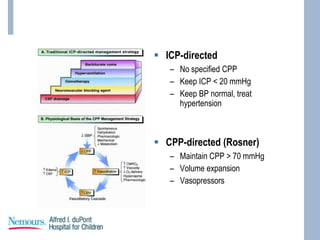
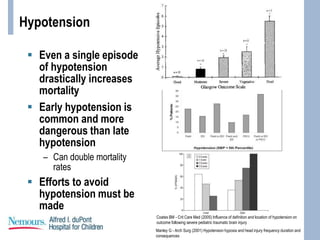
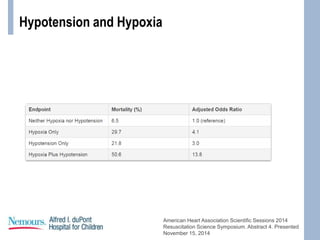
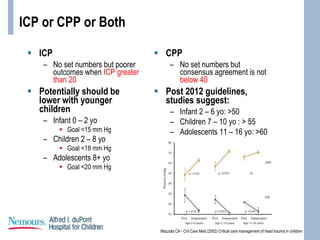
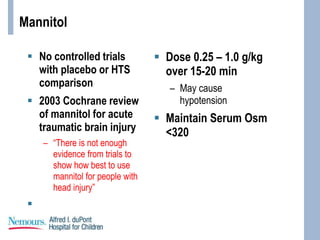
This document provides an overview of pediatric traumatic brain injury (TBI) management. It describes the case of a 13-year-old male involved in a motor vehicle collision. Key goals in management include maintaining cerebral perfusion pressure, decreasing intracranial pressure, and preventing secondary injury. Early management focuses on airway protection, oxygenation, imaging, and treating hypotension and elevated ICP. Refractory elevated ICP may be treated with osmotherapy, barbiturates, or decompressive craniectomy. Ongoing intensive care involves careful monitoring and treatment of ICP, CPP, seizures, and other complications. Outcomes depend on age, injury severity, and development of secondary insults like hypot
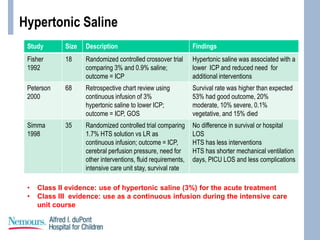
![Hypertonic Saline
Mechanism:
– Rheologic effect
– Osmotic gradient
Proposed additional
benefits:
– Restoration of cell
membrane potential
– Inhibition of
inflammation
– Enhancement of
cardiac output
Dose:
– 3 – 5 ml/kg of 3%
Can push serum
Osm to <360
Can push [Na] to
>160
May be beneficial if
CSW occurs](https://image.slidesharecdn.com/pediatrictraumaticbraininjurypresentationupdated-200402152014/85/Pediatric-traumatic-brain-injury-presentation-35-320.jpg)