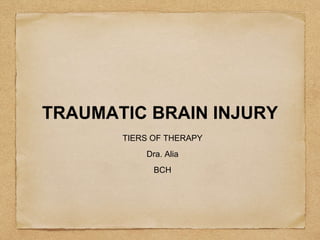
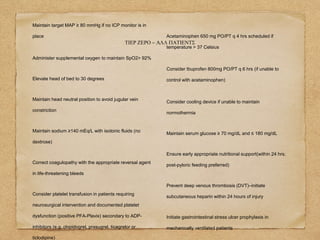
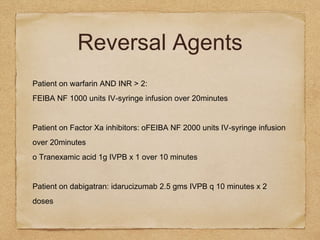
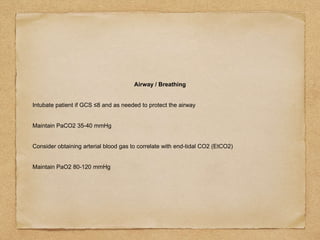
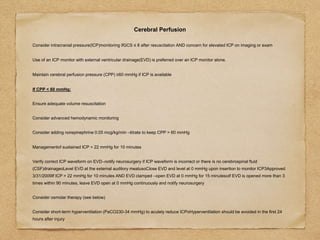
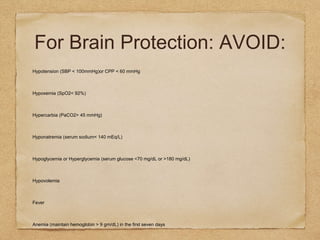
This document outlines a tiered approach to the management of traumatic brain injury. Tier Zero outlines basic care for all patients, including maintaining blood pressure, oxygen levels, head position, sodium levels, and preventing complications. Tier One adds more aggressive interventions for patients with GCS ≤8, such as intubation, ICP monitoring, osmolar therapy, and sedation/analgesia. Tier Two considers additional osmolar therapy and interventions if ICP remains elevated, while Tier Three involves surgical options and barbiturate coma if more conservative measures fail. The goal at each tier is to maintain cerebral perfusion pressure and control intracranial pressure.