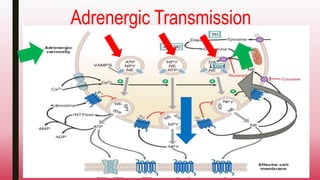
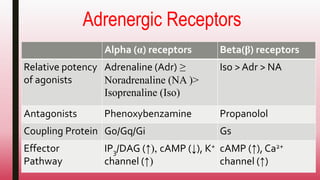
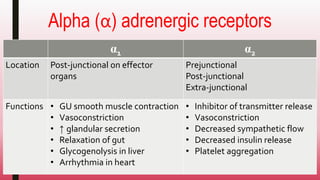
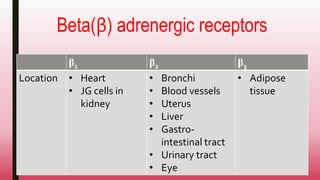
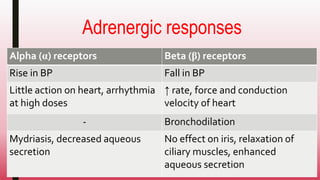
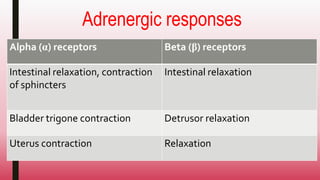
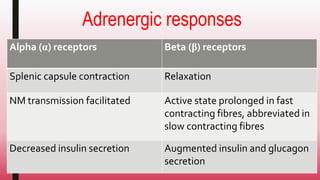
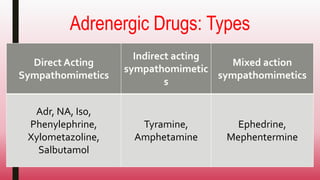
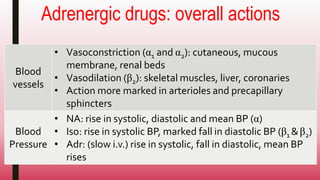
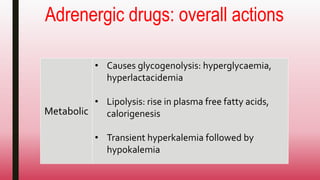
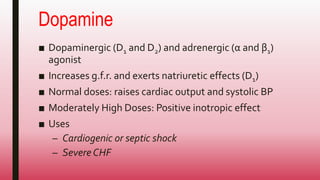
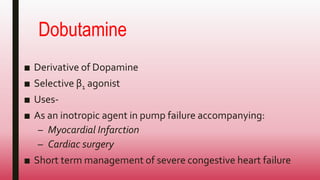
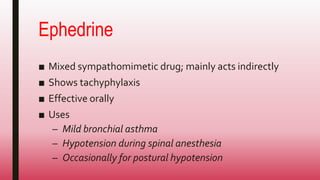
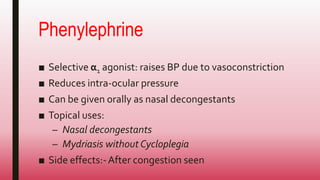
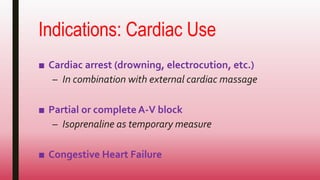
This document discusses adrenergic drugs and their uses. It defines alpha and beta adrenergic receptors, their locations, and functions. Examples of direct and indirect acting sympathomimetic drugs are provided along with their overall actions on the heart, blood vessels, blood pressure, respiration, eyes, and metabolism. Specific drugs discussed in more detail include adrenaline, dopamine, dobutamine, ephedrine, and phenylephrine. Therapeutic uses of adrenergic drugs are outlined for conditions like hypotension, cardiac issues, bronchial asthma, mydriasis, uterine relaxation, attention deficit disorders, and obesity.