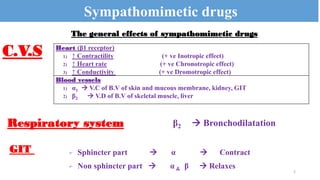
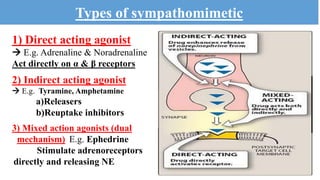
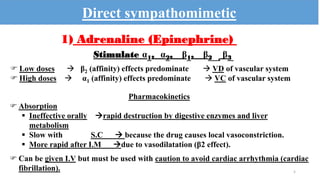
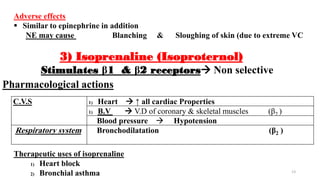
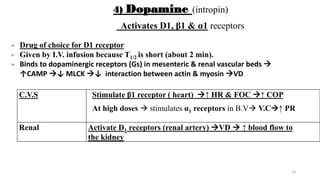
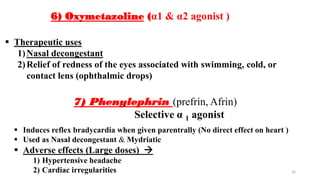
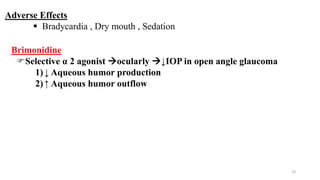
This document summarizes the effects of sympathomimetic drugs. It describes how these drugs act on various receptors in the cardiovascular system, respiratory system, gastrointestinal tract, genitourinary tract, eyes, and metabolism. It provides examples of direct-acting agonists like adrenaline and noradrenaline, indirect-acting agonists like tyramine and amphetamine, and mixed agonists like ephedrine. It discusses the therapeutic uses and adverse effects of various sympathomimetic drugs.