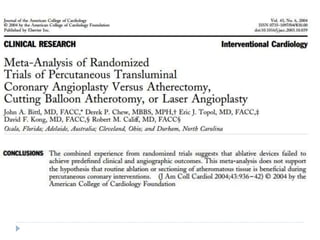
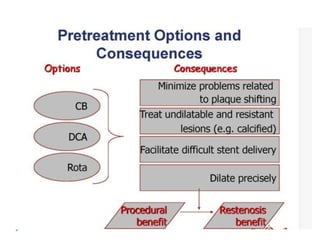
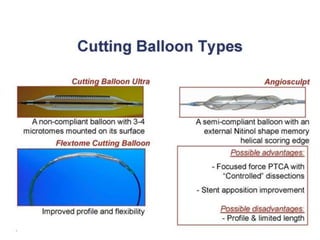
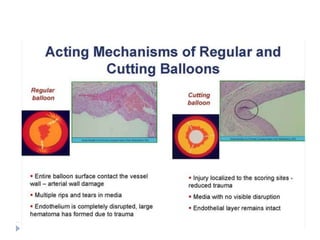
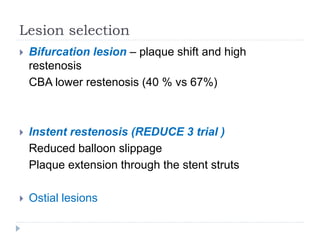
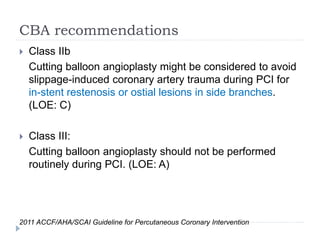
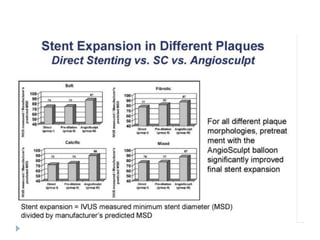
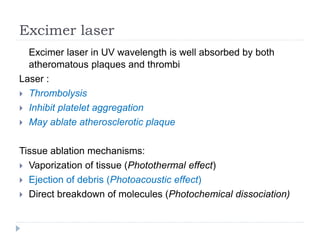
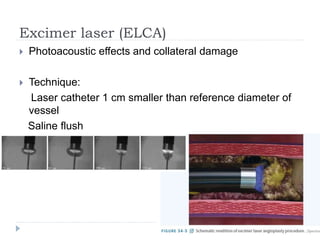
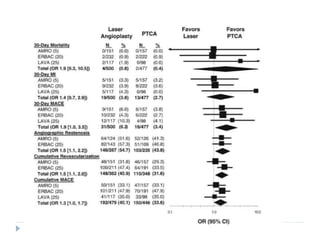
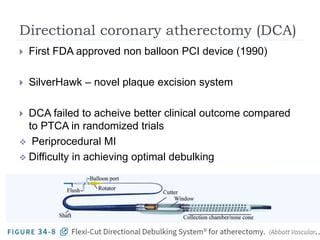
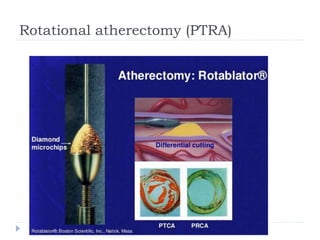
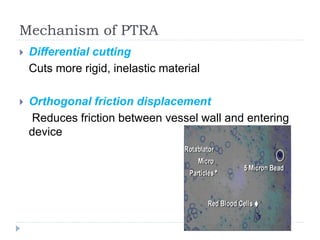
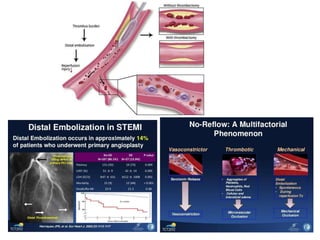
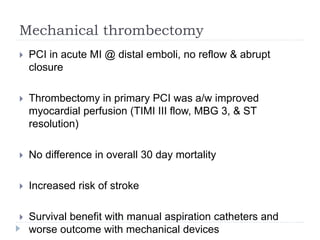
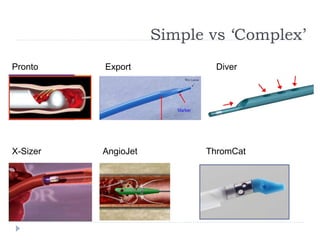
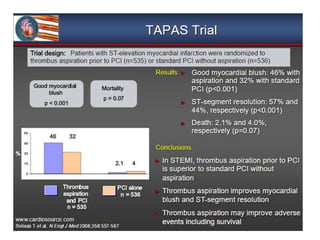
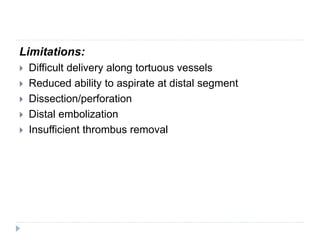
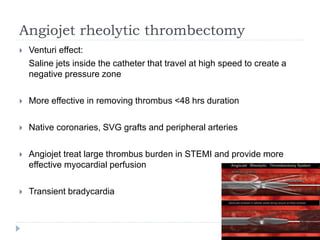
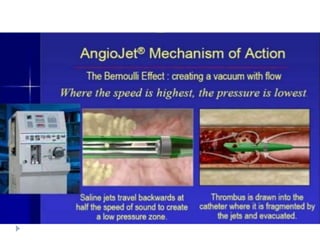
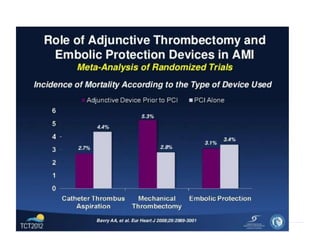
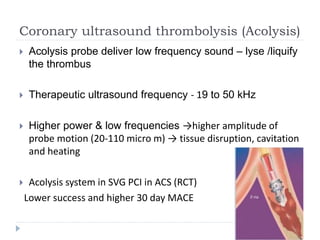
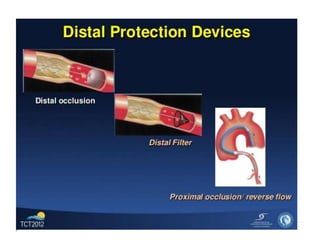
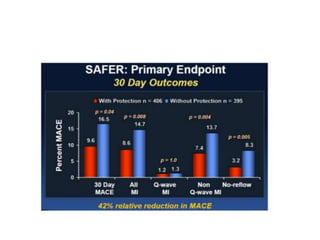
This document discusses various adjunct devices that are used in percutaneous coronary interventions (PCI). It describes plaque modification devices like cutting balloons and lasers that can facilitate procedural success and reduce restenosis. Cutting balloons make controlled incisions in plaque to enlarge vessels at lower pressures. Lasers precisely remove plaque but are infrequently used due to high cost. Thrombectomy devices like manual aspiration catheters can reduce thrombus burden in acute myocardial infarction to improve perfusion. Embolic protection devices trap debris during stenting of saphenous vein grafts to prevent distal embolization.