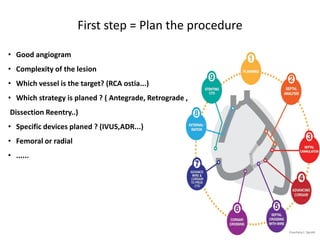
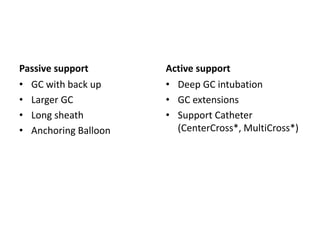
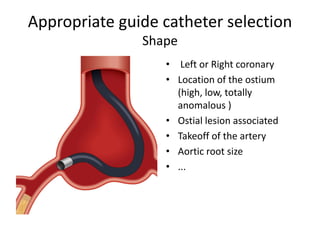
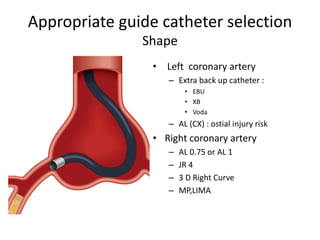
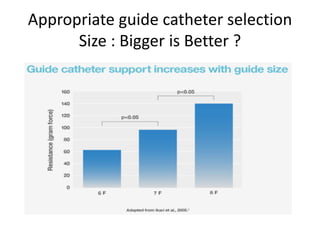
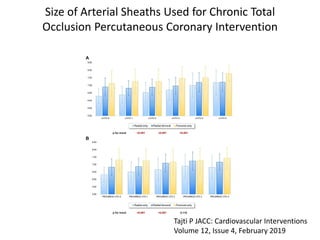
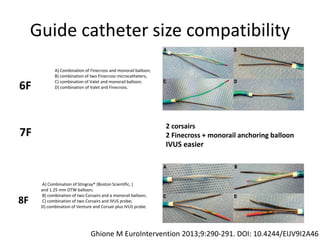
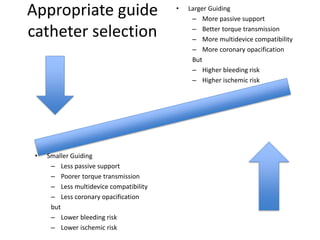
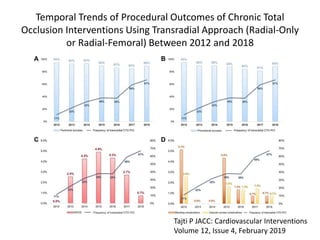
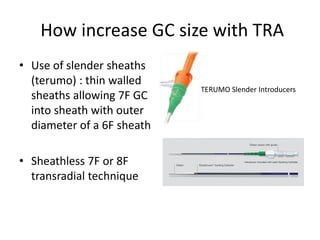
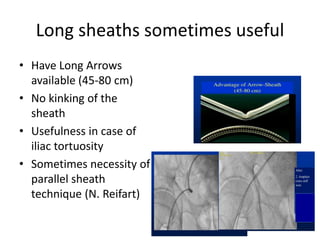
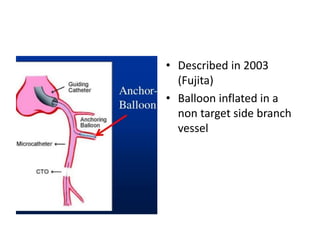
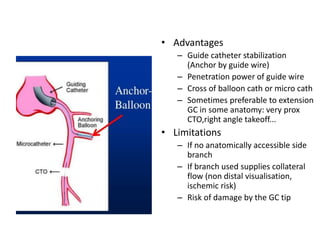
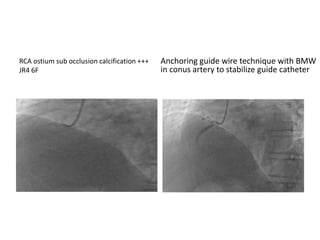
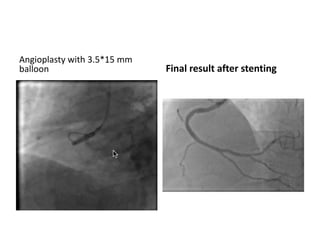
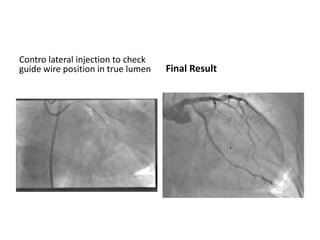
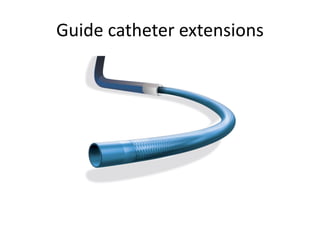
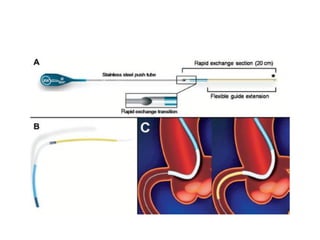
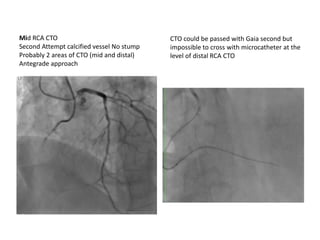
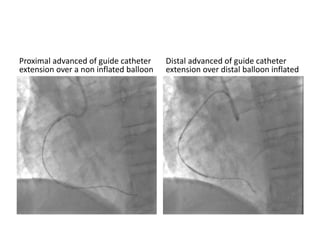
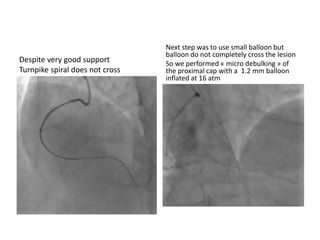
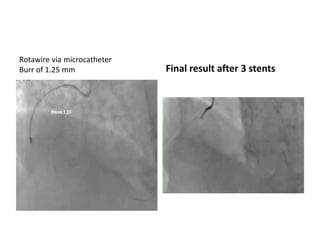
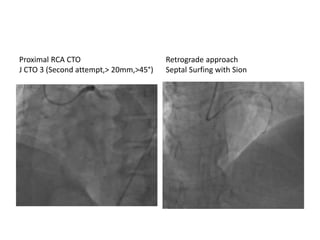
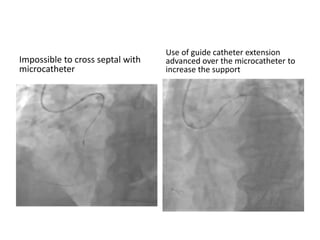
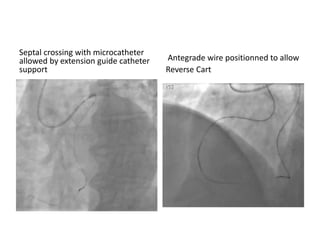
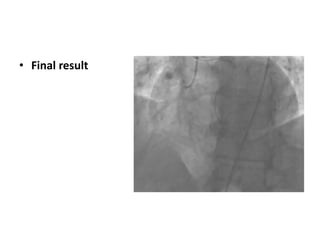
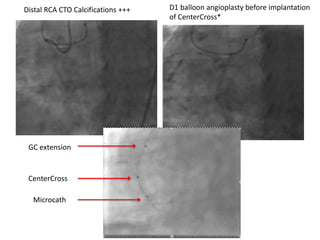
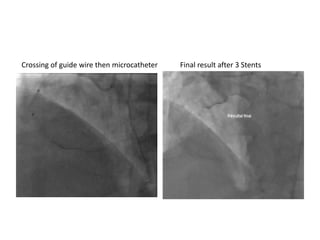
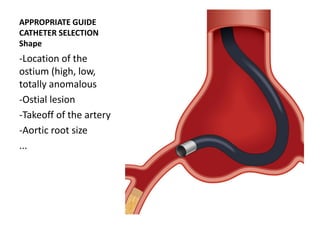
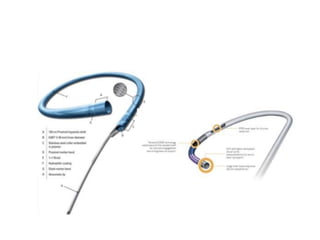
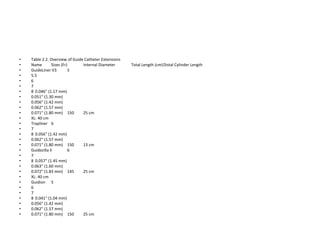
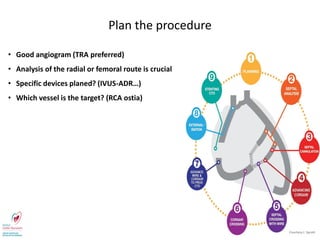
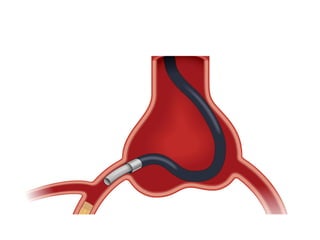
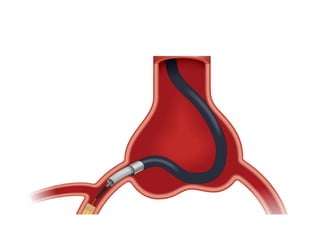
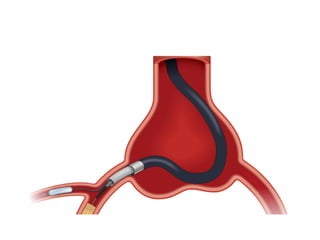
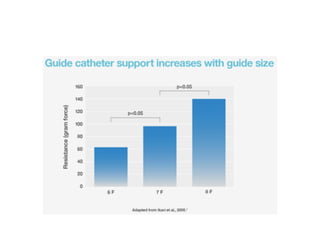
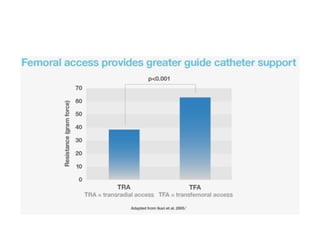
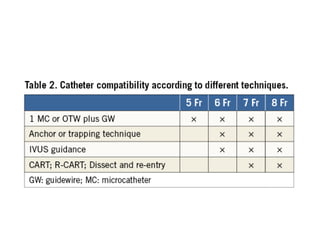
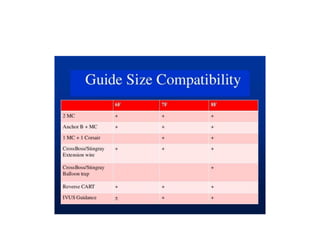
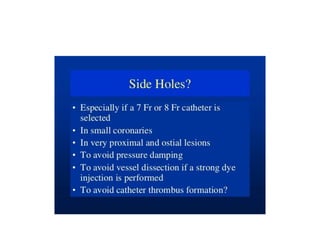
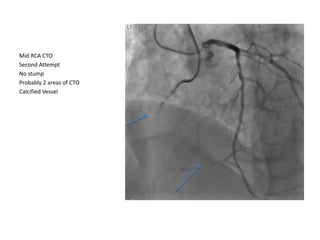
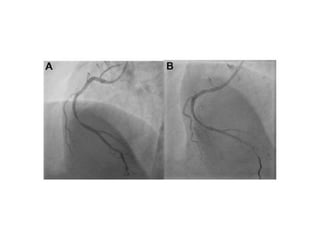
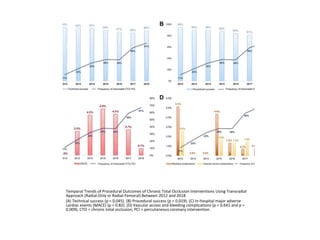
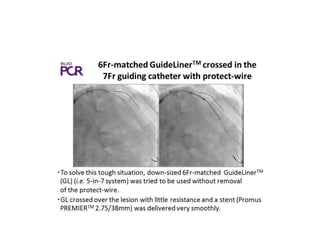
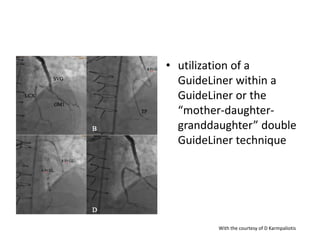
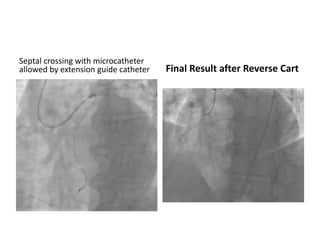
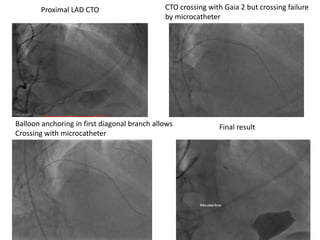
The document provides a comprehensive guide on optimizing catheter support for chronic total occlusion percutaneous coronary intervention (CTO PCI), emphasizing the importance of careful planning and appropriate device selection. It discusses the advantages and disadvantages of various guide catheter sizes and techniques, including passive and active support methods, anchoring balloons, and guide catheter extensions. Additionally, it highlights procedural trends in CTO interventions using transradial access and the necessity of anticipating tools required for successful outcomes.